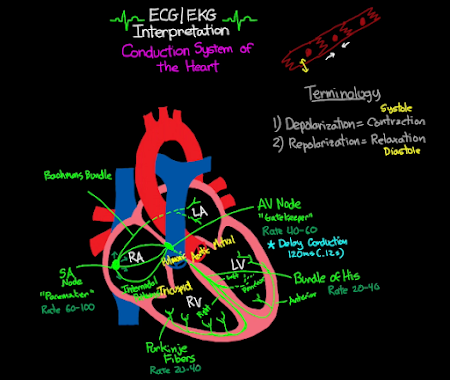
SA node > AV node > Bundle of His > Purkinje fibers
SA 60 - 100
AV 40 - 60
Ventricles 20-40
Bundle of HIS 10-40
Purkinje 20-40
alright guys so yesterday we talked
about the diagnosis and evaluation of
wide complex tachycardias namely
ventricular tachycardia versus svt with
the barrency and today we're going to be
talking about management of ventricular
tachycardia because it's going to happen
very frequently when you're on the wards
or you have cardiology patients so let's
Diagnosis
just get right into it so let's say that
you identify a patient is having
ventricular tachycardia well the first
step that you want to do at this point
is to find whether this is non-sustained
ventricular tachycardia or sustained
ventricular tachycardia if it's less
than 30 seconds then it's non-sustained
v-tac and if it's greater than 30
seconds then it's sustained the reason
this is so important is because
constantly when you are having your
patients you're going to be getting
paged because patients are going to be
having five beat runs of vtec or 10 beat
runs of vtec and basically what you need
to know is that this is non-sustained
vtec and it's treated much differently
than if it's sustained monomorphic vtac
in these patients you can then classify
them as are they asymptomatic or are
they symptomatic in both cases i would
check electrolytes because a lot of
times if the patient's electrolytes are
really out of whack then it's a really
good idea to just replace those
electrolytes and make sure they're in a
good range so that the risk of them
having runs of vtac is significantly
diminished but otherwise if they're
asymptomatic you really don't have to do
anything in this case if they are
symptomatic then at this point you would
initiate a beta blocker or a calcium
channel blocker if they continue to be
refractory then you may decide to do
amiodarone and then finally if that
continues to be refractory then you may
start pursuing catheter ablation of
their vtac one side note that i want to
Side Note
mention are a couple things about pvcs
and vtac so basically anytime you have
three or more consecutive pvcs that is
what is called vtac another good number
to know is that if anybody is having
greater than 10 of their heartbeats are
as pvcs then this greatly increases the
chance that they're going to start
having some deleterious cardiac
remodeling from that and that may lead
you a little bit more towards wanting to
do something about it even if they're
asymptomatic there's also
certain rules
of malignancy that you should know about
which predicts the chance of a pvc
causing a significant run of v-tac and
this is called the rules of malignancy
and kind of the important ones to know
here is going to be frequent pvcs
multi-form pvcs so they're kind of
originating from different foci and then
also what's known as the r on t
phenomenon
which is basically when your pvcs are
kind of hitting right on the t wave of a
normal qrs complex and that has a
specifically high propensity for
generating a run of vtac alright so
that's basically it for the discussion
of non-sustained vtec most of the time
when you're going to get paged by the
nurses there's really not that much for
you to do check their electrolytes make
sure they're all replaced correctly if
they're asymptomatic don't really do
anything if they're symptomatic make
sure they're on a beta blocker or
calcium channel blocker now let's talk
about sustained monomorphic vtac and
here you're also gonna split it up into
two kind of categories so first of all
it's gonna be are they stable or are
they unstable and if they're unstable
then you're basically immediately going
to electrically cardiovert them or shock
them if the patient is awake and you can
Treatment
do a synchronized cardioversion then you
can do a hundred joules but honestly if
the patient is significantly unstable or
they're if they're pulseless then you
just want to start directly with a 200
joule shock and then you can up titrate
to like 300 joules and then up to a max
of 360 joules so that's pretty much the
easy treatment for unstable sustained
monomorphic vtac now what if the patient
is stable but they're having this
continuous sustained vtec what's our
treatment here so directly the answer is
going to be we're going to start with
antiarrhythmic therapy there's multiple
options here but the most common one
you're probably going to see is
amiodarone and the way that you do this
is a 150 milligram bolus over the first
milligram per minute rate of a drip for
the next six hours other options include
lidocaine 1 to 1.5 milligrams per
kilogram or procainamide 20 to 50
milligrams per minute so how do you
choose these i would say most people are
probably most comfortable with ordering
amiodarone and that's kind of the
default choice that most people will
have
the things with amiodarone are that it's
a little bit slower onset than the other
medications but it does have a higher
chance of actually reversing the
ventricular tachycardia and it actually
decreases the rate of recurrence of
ventricular tachycardia as well so it's
a very solid option the advantage of
lidocaine is that lidocaine generally
causes the least amount of hypotension
out of all three of these agents and
also potentially has a benefit in the
setting of mi the problem with lidocaine
is that it only fully reverses the vt
about 10 to 20 of the time so really
kind of a low rate of reversing the
ventricular tachycardia and then finally
you have procainamide which reverses the
ventricular tachycardia about 50 of the
time so pretty good rate there and also
has the benefit that even when it
doesn't
reverse the ventricular tachycardia it
actually slows the rate down which is
significantly beneficial as well so
those are some of the three different
options and some of the three different
reasons that you would choose uh them
amongst each other based on their
different side effect profiles and
different efficacies but in general i'd
say you should probably just start with
amiodaro it's the simplest and easiest
and most default one that most people
are going to do one thing to know is
that if the vt terminates during the
infusion you can actually stop the
antiarrhythmic therapy unless it starts
to have a recurrence again in which you
should initiate the infusion again and
then finally if they're refractory and
even despite your antiarrhythmic
infusion they're still staying in
sustained vtac then the next step would
actually be to shock as well and finally
one last thing to note is that there's
something called vt storm and there's
also something called incessant vt and
so vt storm is if you get somebody out
of ventricular tachycardia but they end
up having three or more recurrent
episodes within 24 hours then you call
that vt storm if you also have vt that
recurs within five minutes of
terminating the vt that's also called vt
storm as well and finally
incessant vt is basically when you have
vt that lasts for hours even though the
patient's hemodynamically stable then
you can call that incessant vt in either
of these scenarios if the patient is on
amiodarone or an antiarrhythmic already
then you should also add on a beta
blocker sometimes apparently propranolol
because apparently it's been shown to
have an increased efficacy of
terminating vt
but they should be on a beta blocker at
this point if they aren't already so
yeah that's my quick and simple way of
deciding how to treat ventricular
tachycardia number one is really to
identify is this non-sustained
ventricular tachycardia or is this
sustained ventricular tachycardia and
then from there you really decide how
you're going to treat the patient based
on their symptoms or if they're stable
or unstable so i hope that quick video
Outro
was very useful for you if you didn't
see the first video on evaluating and
diagnosing wide complex tachycardias
especially uh regarding differentiating
svt with aberrancy and vt then click up
over here for that video thanks again
for watching this video i know it was a
simple one but i think it was also a
useful one that warrants its own short
discussion i'll see you in the next
video and peace



Comments
Post a Comment