Intermediate stress failed. concrete questions why you are calling
22F candidate inpt stress verse cardiac cath.
within 90 minutes
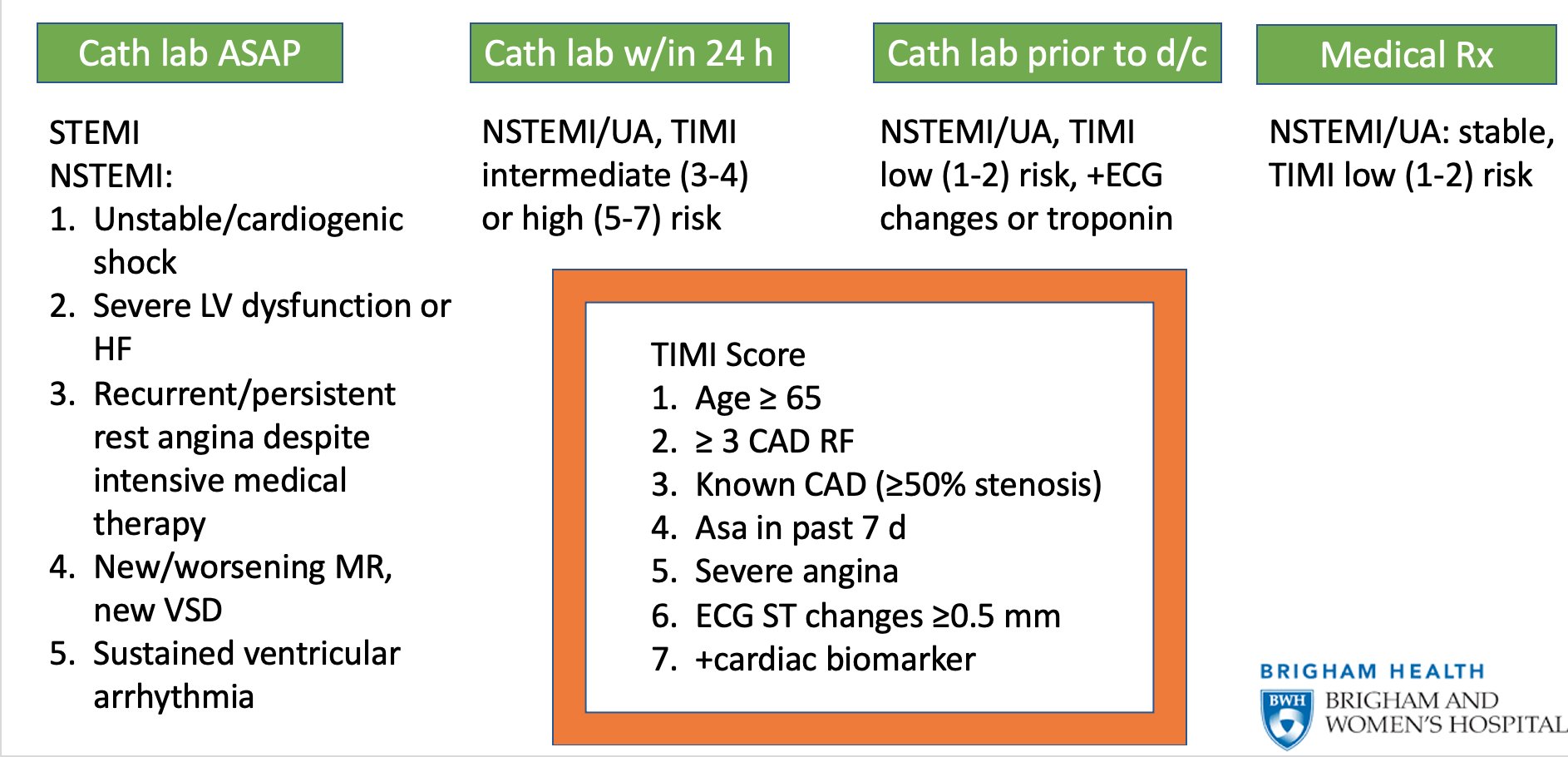
NSTEMI/UA, TIMI intermediate (3-4), high (5-7)
NSTEMI ST elevation
Elevated troponins, chest pain, EKG changes
any 2 of the 3 NSTEMI
Unstable angina
DAPT: asa, statin, heparin,
oxygen, ace inhibitors, beta blockers, don't give oxygen
give them O2 only for hospitalists via small mechanical fan.
morphine grade 2b.
STEMI: loading DAPT, +/- heparin, go straight to cath lab.
not in cath lab, thrombolytic. TNK: tenectaplase.
Jama Clinical Reviews
- STEMI cardiac cath w/in 2 hours
STEMI no PCI
- Fibrinolcytics Alteplase, reteplase, tenecteplase, streptokinase
- PCI w/in 24 hours
Cath obstructions STEMI in 2 hours do PCI, if NSTEMI then 24048 hours do cath
NSTEMI
- elevated troponin - NSTEMI
- No elevated troponin Unstable Angina
When to treat w/ PCI
STEMI w/in 2 hours
NSTE-ACS w/in 24-48 hours
NSTEMI
High sensitivty troponins yes NSTEMI
No Unstable angina
| Cause | Type of ACS | Pathophysiology | Characteristics | Percentage of ACS |
|---|---|---|---|---|
| Plaque rupture | STEMI or NSTEMI | Lipid-laden plaque rupture due to inflammation followed by development of platelet-rich thrombosis | Most common etiology in both sexes<br> | Approximately 60% |
| Plaque erosion | STEMI or NSTEMI | Plaque erosion occurs with local flow perturbation, resulting in a denuded endothelial surface with formation of neutrophil extracellular traps and propagation of thrombus formation | More common in women than in men | Approximately 25% |
| Calcific nodule | STEMI, NSTEMI, or UA | A protruding nodular calcification penetrates the lumen surface with subsequent thrombus formation | Patients with chronic kidney disease and those receiving dialysis have a higher prevalence of coronary calcific nodules; calcific nodules are associated with a higher rate of requiring repeated coronary revascularization due to growth of the calcified nodule<br> | Approximately 5% |
| Coronary spasm | STEMI, NSTEMI, or UA | Extreme vasoconstriction of an epicardial coronary artery, which causes near-total or total vessel occlusion and sometimes superimposed thrombosis; can also occur in the microvasculature | In patients with ACS who do not have obstructive coronary artery disease on angiography, coronary spasm can be evaluated with provocative testing, such as administering acetylcholine, although it is typically treated empirically without such testing | 1%-5% |
| Spontaneous coronary artery dissection | STEMI or NSTEMI | Obstruction to blood flow due to an intimal tear as well as separation of the medial and adventitial vascular walls associated with intramural hematoma protrusion into the lumen; either in single or multiple arteries; more often affects the middle and distal portions of the artery, most commonly the left anterior descending artery | Approximately 90% of patients with SCAD are women (approximately 55% are postmenopausal); emotional stress reported in approximately 50% of patients and physical stress in approximately 30% of patients; fibromuscular dysplasia, systemic inflammatory disorders, peripartum state, and connective tissue disorders predispose; best to reserve PCI or CABG for refractory symptoms | 1%-4% |
| Coronary artery embolism | STEMI or NSTEMI | Conditions such as atrial fibrillation, left ventricular thrombus, valvular thrombus, or paradoxical emboli from the venous system passing through an atrial or ventricular septal defect are associated with coronary artery embolism, which leads to complete obstruction of an epicardial coronary artery or branch and infarction of the myocardium served by that vessel | Evaluation with transesophageal echocardiography and continuous electrocardiographic monitoring are useful to evaluate for several of the causes | 1%-3% |
| Myocardial infarction with nonobstructive coronary arteries | STEMI or NSTEMI | Can occur from a variety of causes, e.g., plaque disruption (plaque rupture or erosion and calcific nodules), epicardial coronary vasospasm, microvascular dysfunction, spontaneous coronary artery dissection, coronary embolism, or coronary thrombosis, which lead to MI despite the absence of any severe obstructive coronary artery stenoses, although the specific cause often remains undiagnosed | More prevalent in women (5 times higher odds) and non-White patients (1.5 times higher odds); less likely to have traditional cardiovascular risk factors<br> | Approximately 5%-6% |
from the JAMA Network this is JAMA clinical reviews interviews and ideas
about Innovations in Medicine Science and clinical practice
my name is Dr Gregory Curfman a deputy editor of JAMA and in this JAMA podcast I'll be speaking
with Dr Deepak Bhatt Dr Bhatt is executive director of Interventional cardiovascular
programs at Brigham and Women's Hospital and professor of medicine at Harvard Medical School
he is also a senior physician at Brigham and Women's Hospital
Dr Bhatt Dr Renato Lopes and Dr Robert Harrington have written a review article titled diagnosis
and treatment of acute coronary syndromes which appears in the February 15 2022 issue of JAMA
welcome to the podcast Dr Bhatt it's great to be with you Dr Curfman
now acute coronary syndromes are characterized as sudden reduction in blood supply to the heart
and the syndromes include SD segment elevation myocardial infarction or stemi
non-st segment television myocardial infarction or nstemi and unstable angina the latter
two are often grouped together as non-st segment elevation acute coronary syndromes
each year an estimated more than 7 million people in the world are diagnosed with acute coronary
syndromes including more than one million people hospitalized in the U.S in this podcast we want
to bring our listeners up to date on these common and potentially serious conditions Dr bot to begin
could you please describe the different mechanisms and pathophysiology of stemi and stemi and
unstable angina what is the pathology at the level of the coronary arteries in the three conditions
this is a great question that you've asked and first of all there's a lot of overlap in terms of
the pathophysiology of acute coronary syndromes whether we're referring to stemi and stemi or
unstable angina one differentiator perhaps between stemi and non-st segment elevation
acute coronary syndromes is whether the artery is completely occluded as is typically the case with
st elevation Mi or incompletely occluded this is more often the case with a non-st segment
elevation Mi or unstable angina so even there there can be potential overlap but let me start
first with stemi they're typically the underlying pathophysiology is plaque rupture that is rupture
of an atherosclerotic plaque in the coronary artery most often this is a lipid Rich plaque
a cholesterol-rich plaque with inflammatory cells and heightened degrees of inflammation
triggering plaque rupture when that plaque ruptures and its inner contents are exposed
to blood a thrombus forms typically a fibrin rich and platelet-rich thrombus this is the
underlying pathophysiology of the majority of ST segment elevation myocardial infarctions however
a good proportion of non-encity elevation Mi or enzyme also has a very similar pathophysiology
perhaps in this setting it's a bit more common to have thrombus that is predominantly plate rich
with perhaps a little bit less of a fibrin rich component but there really is a lot of commonality
here however plaque erosion is something that's been recognized in more recent years as a cause
of acute coronary syndromes though perhaps a little bit more frequent and end stemi than stemi
and what plaque erosion refers to is having the endothelial surface the covering surface of say
a plaque that gets denuded so plaque erosion often caused by some sort of perturbation in blood flow
and then formation of platelet-rich thrombus but again this could be the cause of stemi but it's a
little bit more common in nstemi than stemi it's also a little bit more common in women than men
now there are other causes as well of acute coronary syndromes calcified nodules can cause
stemi or endstemi or unstable angina and here once more there's lipid Rich plaque encroaching upon
the coronary artery Lumen where blood would be flowing but in this case there's a lot of
calcium that's involved in that plaque and this is potentially important not only from a mechanistic
perspective but if this patient were to end up in the catheterization lab with their acute coronary
syndrome the presence of that calcific nodule can pose some particular technical challenges
there are other etiologies for acute coronary syndromes as well again plaque ruptures the most
common followed by plaque erosion than coronary spasm is a cause of acute coronary syndromes
this is where the smooth muscle that is in the artery constricts it can be focal it
can be multifocal it can be multi-vessel it can involve the epicardial arteries it can involve
the microvasculature and it does appear that coronary spasm if we give provocative agents say
in the catheterization Labs such as acetylcholine is maybe a little more common than we used to
think it was on the other hand most of the time when it's suspected it's treated empirically but
still it's important to understand that it can be a part of the pathophysiology of acute coronary
syndromes either the primary player or sort of a secondary phenomenon say when the endothelium has
been damaged and secondarily there may be spasm and then there may secondarily also be thrombosis
spontaneous dissection is another cause of acute coronary syndromes it may manifest as stemi or
even nstemi but a proportion in particular Rusty elevation am I we now know is due to scad or
spontaneous coronary artery dissection there's certain situations such as in the peripartum
state where it might come up a little more frequently than otherwise and this involves an
intimal tear that is a terror of the inner layer of the coronary artery and that can obstruct the
coronary artery in fact we're still learning a lot about scad including the pathophysiology of scad
there are some that believe that the mechanism is predominantly what I mentioned at tear in the
intima and the creation of a true Lumen where blood is Flowing as it should in a false Lumen
that can then fill with blood and compress or obliterate the artery lumen there's also a line of
thinking that some proportion of the spontaneous coriary dissections are from blood forming from
the adventitial side of things and forming within the adventition media of the artery again leading
to a compressive phenomenon and obliteration of blood flow so we're still learning a lot about the
biology of scad and it's likely the case there's several different forms with different specific
pathophysiologies behind them another cause I'll mention is coronary embolism such as when someone
has atrial fibrillation or a left ventricular thrombus that decides to move and obstruct a
coronary artery so this can cause stemi or nstemi and then finally there's a category called minoka
or Mi with non-obstructive coronary arteries it accounts for about five to six percent of
myocardial infarctions and that basically means in those patients who have a coronary angiogram there
there's no obstructive plaque there might be some mod plaque but no severe plaque and then we assume
that one of the causes I mentioned or some other causes on a rather long list of potential causes
is the etiology of the acute coronary syndrome and sometimes more advanced imaging things like
MRI can help us get it with the pathophysiology might have been what the reason for that Mi with
non-obstructive coronary arteries from Anoka might have been so as you can see there really a variety of different etiologies well that's a great summary thank you very much for that
and just to be clear about the distinction between plaque rupture and plaque erosion do you consider
these to be different degrees of disruption of a plaque or does plaque rupture actually involve
Hemorrhage out of the plaque itself and does that Hemorrhage contribute to coronary thrombosis
so it's a great question plaque rupture more often results in complete arterial occlusion
as with a stemi whereas plaque erosion may be more likely to lead to non-obstructive acute coronary
syndrome such as a non-state segment elevation Mi and for reasons that aren't totally clear it
appears that plaque erosions a bit more common in women than men with the reason for that is I think
is something that will need to be elucidated in the earth to come that might provide some insights
into why there may be some subtle differences in ACS presentations and trajectories after
presentation men versus women the biology is a little bit different in as much as plaque erosion
is more a response to the endothelium being disrupted or denuded whereas plaque rupture as
you said is more a matter of exposure of the inner contents of the plaque to the flowing blood and
can include such things as enter plaque Hemorrhage as well so there are some differences if one looks
at autopsy specimens for example between these two there's also some potential implications for
management in general plaque rupture that presents clinically is going to be treated if it's a stemi
with a stent in most regions of the world or in regions of the world whether that's not possible
with fibrinolytic therapy therapy directed towards breaking down the fibrin rich thrombus whereas for
plaque erosion say in an end stemi they're in fact fibrinolytic therapy has been found to be
not useful in fact harmful in terms of causing bleeding complications with no benefit and it
does appear that a higher proportion of patients with plaque erosion may end up doing fine managed
medically without stenting as opposed to those with plaque rupture where stenting does seem to
be particularly useful so there are some definite differences in the pathophysiology and they do
have implications for the treatment some of which has been fully worked out some of which really
does need more research all right thank you for that now I wonder if we could turn to the clinical
presentation of acute Corner syndromes and are there differences in the clinical presentations
among the three types of acute coronary syndromes I wonder if you can discuss that for a moment
this is really a key point that you've raised for anyone directly involved with patient care
understanding the pathophysiology is important for present care it's important for future research
but understanding the differentiation among these acute coronary syndromes that's critical
for right now for today in managing the care of patients with ACS so the first step in a patient
with suspected ACS assuming that they're in an emergency setting if they're calling from home
or somewhere else they need to call Emergency Medical Services 9-1-1 in the U.S and be brought
immediately to an emergency department but then within 10 minutes of arrival the standard of care is to get an ECG or electrocardiogram and there are the key thing to look for is whether
ST segment elevation is present or is not present on the ECG if it is present on the ECG that is a
stemi rst segment elevation myocardial infarction that means everything needs to kick into high gear
the system needs to move quickly that is a medical emergency and time is muscle as they say it really
matters to move quickly here so that's a very important diagnosis to make and we'll talk about
the treatment later but that ECG is key for that differentiation if SD segment elevation is not
present well then it is a non-st segment elevation ACS and that broadly speaking is then divided into
n stemi non-st segmentation Mi or unstable angina again the key differentiator here between stemi
and non-stemi type ACS is the ECG and whether St elevation is or is not present so now here for the
non-sd segmentation ACS there's no SD simulation present the next step is to check a troponin level
preferably a high sensitivity troponin level and if that is elevated initially or on subsequent
testing then the diagnosis of nstemi is made if on the other hand that troponin level is negative
and remains negative on subsequent testing then the diagnosis of unstable angina is made so it
really matters a lot what that electrocardiogram shows and then in the case of non-sd segmentation
ACS with that initial triple opponent shows or subsequent requirement and in terms of subsequent
troponin most algorithms would say within three hours is when that subsequent troponin should be
drawn the most recent data actually suggests an algorithm of checking again in one or two hours
is probably even more efficient with no loss of sensitivity or specificity so I think the
way to get to stemi and stemi-unstable angina is quite clear with use of the electrocardiogram and
with use of the troponin now of course this is all in patients who've presented with a clinical
syndrome that's consistent with ACS and we should talk about that a bit in terms of the symptoms
but in terms of the broad classifications this is how to classify patients into the different types
of acute coronary syndromes excellent well you brought up symptoms so why don't we talk about
symptoms which sometimes can be very classic but other times maybe not so much can you comment
about that absolutely so chest discomfort at rest is the most common presenting symptom of acute
coronary syndromes there's no question about it and everything that I was talking about in terms
of the categorization of ACS applies to patients presenting with a high pre-test probability of
having an ACS so they're presenting with chest discomfort I'm not referring to say troponin
measurements that are done in the hospital for a variety of other reasons where the presenting
symptom is something else or there's no symptom even in that circumstance troponin elevation
is a bad prognostic sign but that isn't really what we're talking about today in terms of ACS
and how to manage acute coronary syndrome so chest discomfort in both men and women is the
most common presenting symptom but it's important to realize that a significant number of patients
will have other less specific symptoms such as dyspnea which can occur in isolation although more
commonly still occurs with there being some sort of chest pain I think in Prior years there's been
lots of talk about atypical chest pain the most recent American College of Cardiology American
Heart Association chest pain guidelines that just came out at the end of 2021 actively discourage
the use of that term atypical chest pain and the reason is not just to be the workplace but to make
sure that treating Physicians realize that that nomenclature can sort of lead us down Pathways
that aren't useful the historical thinking perhaps being that women are more likely to have atypical
chest pain for example but it turns out that's really not true Studies have shown I'll quote one
particular study but there are several now that approximately 79 percent of men and 74 percent
of women presenting with acute coronary syndromes have chest discomfort at rest as their predominant
presenting symptom so yes you could say oh that's more common in men than women but 79 versus 74 to
me is a relatively small difference not clinically actionable so again the majority of men and women
with ACS are presenting with chest discomfort at rest now what about the what used to be called a
typical symptoms such as dyspnea well it turns out that in the particular study I was quoting
for example 48 of women did have non-specific symptoms but guess what so did 40 of men so again
these so-called non-specific previously perhaps called atypical symptoms are occurring in women
that's true but they're also occurring in men but more importantly in both the women and men
even if they are having these non-specific symptoms still a lot of them are also having
chest discomfort they might lead by saying oh yes I'm having really bad shortness of breath but then it turns out they are also having chest discomfort so the history is in all things
remains very important when such a history that's concerning of these sorts of symptoms of chest
discomfort chest pain chest pressure uh dysmia Etc are occurring at rest and are significant well ACS
should be suspected and then we need to launch into the algorithm that you and I just reviewed in terms of ECG within 10 minutes and then High sensitivity troponin testing shortly thereafter
so let's say we now have a diagnosis and we want to move quickly on to treatment
and the treatment of the three types of acute coronary syndromes has advanced substantially
in recent years and there is overlap among therapies for the three categories of acute
coronary syndromes treatment might be broadly categorized into reperfusion therapies on the
One Hand In Medical therapies on the other and if we could begin with stemi
I wonder if you could please discuss the recommended steps in the management of stemi
absolutely this is really important to know because time matters as I alluded to before so all the patients presenting with ACs of all three types should be treated with anti-platelet
and anticoagulant therapy on presentation in a minimum this is typically off an aspirin
and unfractionated heparin but there could be more in terms of antiplatelet or anticoagulant
therapy but then the key sort of determination as I mentioned is the ECG and if there's St
elevation it's time to activate that is called the cardiac catheterization lab if there is a
catheterization lab that's available within two hours data show that's the way to go take that
patient of the cath lab with the stemi and more often than not there's an obstructed epicardial
coronary artery open it up typically with a stent and that is the treatment of choice now if there
isn't a catheterization lab available within two hours because there's a blizzard or because it's
a part of the world where there aren't cath Labs that are as commonly placed well then the best
thing to do is to treat promptly with fibrinolytic therapy or thrombolytic therapies it used to be
called and there are altar plays where the plays or connected plays or the Agents of choice but
if cost is an issue in that particular region of the world streptokinase remains an option as well
for fibrinolytic therapy even in those patients treated with Linux they should then be transferred
to a facility that can perform percutaneous corn intervention within the next six to 24 hours or so
great now in terms of end stemi are there any important differences between the management of
nstemi and stemi it's a terrific question in general it's felt that the timing is
urgent but not quite as emergent as with stemi but that can sometimes be misleading because sometimes
nstemi's or stemmies in Disguise so for example the left circumflex artery and occlusions that
are notorious for not presenting with ST segment elevation same sort of situation with a large
diagonal Branch off the left anterior descending artery where there may not be SD segment elevation on the 12 lead surface ECG but in fact there is an occluded artery so in patients that are having an
nstemi that appear to be high risk such as those with ongoing chest pain despite initial medical
therapy marked ST segment depression that is new and persists if an echocardiogram is done in the
emergency department a patient with a presumed new wall motion abnormality those patients should be
treated just like an st signal Ovation Mi patient in terms of going to the cath lab emergently
but in the majority event stemi cases where that's probably not going to be the case there
you still want to move quickly typically the guidelines would say within 24 to at most 48
hours or so to get that patient to the cardiac catheterization lab assuming that they don't
have any contraindications and then based on the coronary Anatomy undergoing revascularization
about 60 or so patients will end up getting a coronary stent about 10 or so will get coronary
bypass surgery during that index hospitalization and the remainder will be treated with medical
therapy only of course all the patients will be treated with medical therapy and be given lifestyle modification recommendations on discharge but specifically the ones who have
severe blockages will be treated percutaneously or with surgery so that's the management of
nstemi in general though low risk and stemi or unstable angina can be managed medically as well
as the the initial therapy where the medicines I mentioned are given but additionally medicines
directed towards controlling ischemia things like beta blockers but also other risk factor control
medicines lipid lowering therapy Etc employed and if the patient continues to have symptoms
then they would go on to the catheterization lab in that more so-called conservative strategy
where initial medical therapy only is utilized or there it would make sense to also do early on some
sort of non-invasive evaluation historically that's been stress testing but more recently
in areas where it's available non-invasive computed tomography angiography or CT angio
has really caught on as a quick way to exclude severe coronary disease that is if that comes
back looking pretty normal it's unlikely that the patient has an ACS whereas if that comes
back looking like there's severe coronary artery disease or it's a bit ambiguous then the patient will likely undergo cardiac catheterization anyway so there is I think a lot more subtlety to the
management of non-sd segmentation ACS than there is of stemi with a few different Pathways that are
possible but in general patients that are higher risk even those that have unstable angina with
negative troponins if they've got things such as heart failure Dynamic ECG changes ongoing chest
discomfort any sign of hemodynamic instability there again prompt catheterization and if
appropriate based on the anatomy revascularization would be indicated great thank you very much now
I wonder if there's any specific guidance that you'd offer Physicians as they provide longer term
care and follow-up for their patients with acute coronary syndromes what potential complications
should Physicians be especially mindful of during that longer term follow-up period this is really
an important aspect of the care of the patient with ACS so far we focused in this conversation
on the early care that's critically important of course what the long-term care is as well
data such as from the reach registry published in Jama some years ago showed that in patients with
atherosclerosis if they had a history of Prior Mi and I'll generalize here to say prior ACS
they have a substantial rate of recurrent ischemic events about 20 percent or so at least will have
an ischemic event such as cardiovascular death the my stroke in the next four years or so so
these are high risk patients even if they've done well initially it's important to recognize that
it's important to provide counseling regarding lifestyle modification including things such as
smoking cessation or vaping cessation or cessation of use of any sorts of tobacco products important
to council against drug abuse or proportion of Mis are due to things like cocaine or amphetamine or
opioid use or even marijuana that many Physicians actually don't know of that relationship between
marijuana use and myocardial infarction so important to counsel patients against using
all those different substances for those that are overweight weight loss would be important a diet I
would say in particular diet that is plant-based I would generally recommend and daily exercise
is another important part so all of this I think is easiest to Institute by referral to a formal
cardiac rehabilitation program that remains quite under utilized in the United States and worldwide
but I think every patient with ACS should at least be offered that possibility of cardiac
Rehabilitation where all the different lifestyle measures and more can be implemented beyond the
lifestyle aspect then there's medical therapy so the majority of patients being discharged with acute coronary syndromes should be discharged on Dual anti-platelet therapy that means aspirin
typically low dose aspirin in the range of 75 to 100 milligrams a day and also an ADP receptor
antagonist and the choices are Clopidogrel project girl or tycagorn probably goes beyond
the amount of time we have to discuss all the issues pertaining to choice of agent there but
the review article does touch upon some of those considerations so dual antiplatelet therapy for
the majority of patients with ACS irrespective of whether that treatment was with a stent or
bypass surgery or medications alone in addition to dual antiplatelet therapy then we want to make
sure that the patients are on potent LDL reducing therapy so by that I mean high intensity statins
for all patients barring true contraindications or intolerances acetamide for many patients is a way
to further lower their LDL cholesterol potentially if the triglycerides are elevated consideration
of lycosapentethyl and then medicines that have been used historically in ACS patients such as
beta blockers and ACE inhibitors or Angiotensin receptor blockers and mineral corticoid receptor
antagonists now there it sort of depends on different things beta blockers are strongly
indicated if there's left ventricular dysfunction or if there's significant residual coronary artery
disease with angina it's not so clear what their utility is if the left ventricular function is
totally normal and the patient has been fully revascularized our ACE inhibitors or arbs are
strongly indicated if there's left ventricular dysfunction or diabetes or if there's just hypertension that needs to be treated and mineral corticoid receptor antagonists specifically for
patients with left ventricular dysfunction so it's a rather long list of things to consider the patient especially the de Nova ACS patient might have come in with no medicines but now they're
going to go out on a lot so we have to consider pill burden and cost and a number of other issues as well but that's the basic list of medications and one should consider Beyond just good control
of hypertension good control in those that have it of diabetes and other cardiovascular risk factors
so there are a lot of therapeutic interventions that need to be considered in patients with acute
coronary syndromes and before we wrap up I just wanted to ask you if you foresee any
new developments in the management of acute Corner syndromes on the horizon
do you anticipate novel advances that Physicians should be watching for
I'm glad you asked in this review article hopefully your readers will see that ACS and
the study of ACS is very Dynamic there's a lot that's already been going on in the field over the past few years over the past several years it's not ACS like it used to be say a decade ago
similarly I think in the next decade we'll see tremendous advances in the field of acute coronary syndromes in terms of what's going on in the catheterization lab further advances in
stent technology further advances in assessing whether coronary lesions are significant and
should or should not be stented further advances in cardiac surgery as well further advances in
medical therapy that would apply to the vast majority of ACS patients were I hope will have
antith thrombotic agents that are not only potent but perhaps less bleeding risk than
what we have available today as well in terms of the lipid axis I think will have even more potent
ways of lowering LDL cholesterol and Associated lipid related and inflammatory biomarkers there
are a number of randomized clinical trials that are going on that are looking at a variety of different agents that Target the lipid axis the inflammatory axis drugs that are diabetes drugs
such as sglt2 Inhibitors that are being studied in post-acs patients so really it's a long list
of medicines that are being studied some are drugs that are being used for other indications
I mentioned the sglt2 Inhibitors others are being developed specifically as novel agents and find
finally I'll just say there's also work going on in terms of remote monitoring of patients so
potentially in the future we'll have a situation maybe using wearables where patients who are at
high risk for ACS such as ones who are already had an ACS are monitored remotely and there's
a trigger that goes off with their wearable their their smartphone or whatever that lets them know
or lets their physician know or lets Emergency Medical Services know that there might be trouble Brewing so I see a lot of advances coming in the next decade in ACS well Dr butt you are a Fountain
of Knowledge on this topic and other topics too so thank you very much for your insightful commentary
on these important clinical conditions thank you very much and thanks to all our listeners
and I want to remind listeners that further details about acute Corner syndromes may be
found in the review article by Dr spot Lopes and Harrington in the February 15 2022 issue of Gemma
this episode was produced by Daniel morrow at the JAMA Network the audio team here also includes
Jesse mccorders Shelly stefans Lisa Hardin Audrey Foreman Marilyn frickle luck and Dr Robert golub
is the Gemma executive Deputy editor to follow this and other Gemma Network podcasts please visit
us online at Gemma networkaudio.com once again I'm Dr Gregory kerfman a deputy editor of Chama


Comments
Post a Comment