Traumatic Brain Injuries / Subarachnoid Hemorrhage / Subdural Hematoma / Intraparenchymal hemorrhage
CNS emergencies
The patient, with a complex medical history, has signs of traumatic brain injury (TBI) and acute subdural hematoma (SDH). Learners will be tasked with prompt and effective management, including assessing the need for coagulation optimization, blood pressure control, recognizing and treating an intracranial pressure (ICP) crisis, and initiating seizure prophylaxis.
Coagulation Optimization:
Review coagulation labs (INR, PTT, fibrinogen, TEG).
Aggressive reversal of therapeutic anticoagulants.
Consider tranexamic acid if <3 hours and moderate/severe TBI.
Blood Pressure Control:
Set initial blood pressure targets based on age.
Initiate norepinephrine infusion if hypotensive.
Resuscitate as needed with blood products or crystalloid.
Recognizing & Treating ICP Crisis:
Identify signs of neuroworsening, anisocoria, or posturing.
Consider empiric hypertonic treatment while awaiting a STAT CT scan.
Seizure Prophylaxis & Diagnosis:
Administer prophylactic levetiracetam.
Consider vEEG for comatose patients with possible seizures.
General Neurocritical Care Practices:
Ensure airway control as needed.
Implement aggressive fever management.
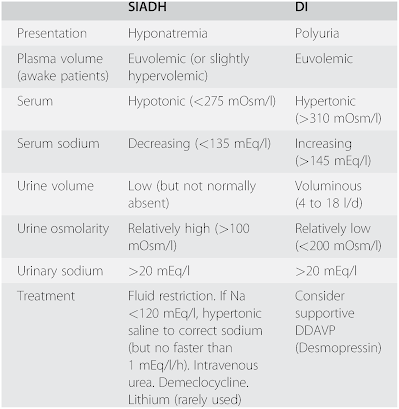
Avoid hyponatremia.
Target normocapnia and maintain a neutral neck position.
Thromboelastography (TEG):
R-Time (Reaction Time): 10.5 minutes (Normal Range: 8 - 12 minutes)
K-Time (Kinetic Time): 4.8 minutes (Normal Range: 2 - 5 minutes)
α-Angle (Alpha Angle): 52 degrees (Normal Range: 47 - 74 degrees)
MA (Maximum Amplitude): 64 mm (Normal Range: 55 - 72 mm)
G (Shear Elastic Modulus): 11 dynes/cm^2 (Normal Range: 9 - 13 dynes/cm^2)
LY30 (Lysis 30): 2% (Normal Range: 0 - 8%)
Interpretation: The TEG profile suggests normal clot initiation, propagation, and strength with mild fibrinolysis.
In the optimal scenario for the presented case involving a 90-year-old male with a history of CHF, CKD, and suicidal ideation, the initiation of a rapid response is marked by the RN alerting the provider to the patient's condition persisting for more than five minutes. The learner promptly undertakes a systematic approach, seeking pertinent information on physical examination, vital signs, and relevant laboratory and imaging findings. Recognizing the severity of the situation, the learner initiates a Stat Neurosurgery Consult to evaluate the potential need for intracranial pressure (ICP) monitoring, external ventricular drain (EVD) placement, or decompressive hemicraniectomy. Collaborating with the neurosurgical attending, the learner engages in a discussion to formulate a comprehensive management plan, including actions such as elevating the head of the bed, administering analgesics, monitoring metabolic parameters, considering mannitol therapy, and initiating antihypertensives as deemed necessary. In parallel, the participant requests an ICU consultation for ongoing critical care. Following a timely response from the consultation, the patient is intubated, and preparations for transfer to the intensive care unit are made, culminating in the conclusion of the case. This scenario underscores the importance of swift and coordinated decision-making in addressing the complexities of traumatic head injury and associated critical care measures.
Blood pressure goal less than 140 To control use IV labetalol or nicardipine drip avoid hydralazine Cleviprex can be used in brain bleeds as it is faster on and faster offset usually is cheaper however price has been increased over time
Correct coagulopathy with INR greater than 1 point can give vitamin K 10 mg IV x 1 and 3 to 5 units of FFP or PCC or Kcentra
To reverse uremia/antiplatelets can consider DDAVP 0.3 mcg/kg IV
To reverse heparin or low molecular weight heparin continues protamine sulfate
After tPA or tenecteplase check the fibrinogen and give cryoprecipitate
For rivaroxaban or apixaban given the excellent health
Keep sodium 1 45-1 55 keep glucose less than 180
Seizure Prophylaxis with keppra loading dose 20mg/kg as a one time dose
then keppra 500 bid
If seizures or status do antiepileptic dosing
Status epilepticus (off-label use): IV: 1 to 3 g as a single dose administered at a rate of 2 to 5 mg/kg/minute (Ref) or 40 to 60 mg/kg as a single dose infused over 5 to 15 minutes in combination with a parenteral benzodiazepine. Maximum single dose: 4.5 g
40 to 60 mg/kg single dose over 5 to 15 minutes in combination with a parenteral benzodiazepine






Comments
Post a Comment