Correct! The gallbladder and the portal vein make an exclamation point, where the gallbladder is the oval, and the portal vein is the circle. Connecting the two structures of this exclamation point is the main lobar fissure, which is typically a hyperechoic line on ultrasound. Recall that the portal vein is apart of the portal triad made up of the common bile duct, portal vein, and hepatic artery.
True Neck stones (stones located in the neck of the gallbladder or cystic duct) are:
-
More likely to be missed on ultrasound because they can be obscured by overlying bowel gas or not fully visualized if the entire gallbladder isn’t scanned.
-
More likely to be symptomatic, as they can block bile flow and lead to acute cholecystitis.
Always ensure the neck is included during your scan and look carefully for the "stone in neck" sign.
Correct! Stones in the neck of the gallbladder can cause more pain. When scanning the gallbladder, ensure you fan through the neck of the gallbladder a neck stone is not missed. Stones may be hard to see, but secondary signs of posterior shadow from the neck, can be indicative of a neck stone. The stone in neck (SIN) sign if when a stone is found in the neck of the gallbladder. SIN was shown in one study to have a specificity of 97% and a positive predictive value of 93% in diagnosing cholecystitis, thus if found is highly predictive of cholecystitis.
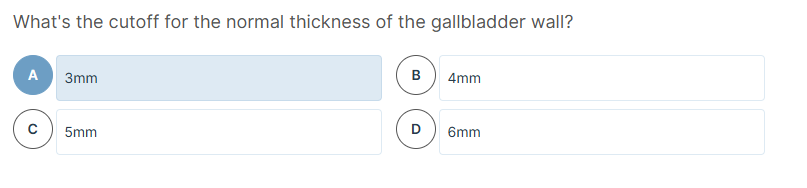
Correct! Normal gallbladder wall thickness is <3mm. Although in cholecystitis, wall thickness is often 5-6mm or greater. Wall thickness is most commonly seen in cholecystitis, however can also be seen in ascites, CHF, hepatitis. Data on why 3mm is a cutoff is limited, but an initial study in 1979 set 3mm as a cutoff. In this study 12 patients had thick walls and cholecystitis, while 5 had thick walls, but no cholecystitis. Therefore, in individuals with gallbladder wall thickness, it is important to assess for other diagnostic criteria for cholecystitis.
Great question — the Tokyo Guidelines (TG18/TG13) provide a standardized framework for diagnosing acute cholecystitis, especially when gallbladder wall thickening alone is nonspecific (as it can occur in CHF, hepatitis, ascites, etc.).
Tokyo Guidelines Criteria for Acute Cholecystitis
Diagnosis is made based on clinical, laboratory, and imaging findings:
A. Local Signs of Inflammation (at least one)
-
Murphy’s sign
-
Right upper quadrant (RUQ) mass, pain, or tenderness
B. Systemic Signs of Inflammation (at least one)
-
Fever
-
Elevated C-reactive protein (CRP)
-
Elevated white blood cell (WBC) count
C. Imaging Findings
-
Gallbladder wall thickening (>3–4 mm)
-
Pericholecystic fluid
-
Gallstones or sludge
-
Sonographic Murphy’s sign
-
Gallbladder distension
Diagnostic Criteria Based on Tokyo Guidelines
| Diagnosis | Requirements |
|---|---|
| Suspected Acute Cholecystitis | One item from A + one item from B |
| Definite Acute Cholecystitis | One item from A, one from B, and C imaging findings |
Takeaway
-
Wall thickening alone is not diagnostic.
-
Combine clinical, lab, and imaging data.
-
Use the Tokyo Guidelines as a structured tool to support clinical decision-making.
it's normal
Incorrect! Although this gallbladder appears to have a thickened wall, only minimal inner lumen is visible. This can be described as a small inner halo, which can be seen during contraction of the gallbladder. This is a normal variant of a gall bladder. The gall baldder is located in the near field, close to the receding edge. This is a contracted gall bladder, where the wall looks falsely thick because it is contracted. No free fluid or shadowing suggesting stones.
Where should you measure the GB?
Cephalad
Caudal
Posterior
Anterior
Correct! Gallbladder wall should be measured anteriorly. Bowel gas and enhancement can interfere with measurement. Measurement is from the entire hyperechoic line of the GB wall. It is important to ensure your probe is perpendicular to the gallbladder, as oblique views can cause falsely elevated measurements of the gallbladder wall.
Correct answer: Anterior
You should measure the gallbladder (GB) wall anteriorly on ultrasound.
Why Anterior?
-
The anterior wall is closest to the probe and gives the clearest, most reliable measurement.
-
The posterior wall may appear falsely thickened due to:
-
Posterior acoustic enhancement
-
Bowel gas
-
Artifact
concise summary of the key learning points from Dr. Joe Minardi’s AEUS narrated lecture on gallbladder ultrasound:
Why Gallbladder POCUS Matters
-
RUQ pain is a common ED complaint, and biliary disease is often on the differential.
-
POCUS is fast and accurate, can reduce length of stay, and expedites diagnosis/treatment.
-
Bedside ultrasound is especially useful in patients with non-specific symptoms, altered mental status, or abnormal liver labs.
Ultrasound Technique Essentials
-
Probe: Curvilinear or phased-array (2–5 MHz)
-
Views:
-
Start subcostal, midclavicular with indicator to head
-
Adjust with deep breaths, intercostal, lateral, or left lateral decubitus positioning
-
Use liver as acoustic window
-
-
Goal: Visualize the entire gallbladder (fundus, body, neck)
Key Anatomical Landmarks
-
Main lobar fissure (MLF): Leads to gallbladder
-
Portal vein: Appears as the "dot" in the exclamation point sign
-
Gallbladder: Anechoic, tear-drop shaped structure with wall <3 mm
-
Common bile duct (CBD):
-
Sits anterior to portal vein
-
<6 mm normal; allow 1 mm per decade over 60
-
Use color Doppler (CBD = no flow)
-
Sonographic Signs of Cholecystitis
-
Gallstones with acoustic shadowing
-
Sonographic Murphy’s sign
-
Wall thickening >3 mm (measure anteriorly)
-
Pericholecystic fluid
-
Sludge (no shadowing, layering)
-
Stone in neck – commonly missed, more symptomatic
-
WES sign (Wall-Echo-Shadow): Gallbladder full of stones
Normal Variants & Pitfalls
-
Contracted gallbladder: Thin with echogenic walls and inner halo
-
Folds & septations: May mimic stones, but no shadowing
-
Edge artifacts: Mimic stones but follow contour, no shadow
-
Bowel loops: Can mimic gallbladder—use MLF, portal vein, and sweeping to differentiate
Performance of ED POCUS
-
High sensitivity/specificity (~85–95%) for cholelithiasis and cholecystitis
-
Comparable to formal radiology ultrasound
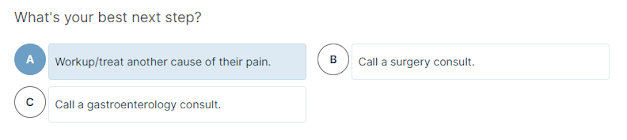
Clinical Algorithm Summary
-
Normal scan: Unlikely cholecystitis → consider other causes
-
Stones only: If stable → outpatient follow-up
-
Abnormal labs or symptoms: Further imaging or admit
-
Multiple signs (stones + wall thickening + fluid + Murphy’s) → Surgical evaluation/admission
Pearls & Tips
-
Use respiratory motion to bring gallbladder into view
-
Be systematic: Always scan fundus, body, and neck
-
Correlate with clinical findings—stones alone may not explain pain
-
Be aware of limitations: patient body habitus, fasting state, bowel gas
True
Normal measurements of the common bile duct (CBD) can be age-adjusted.
Key Points:
-
A normal CBD is typically ≤6 mm in adults.
-
However, after age 60, it's common to add ~1 mm per decade.
-
Example: A 70-year-old may have a normal CBD up to 7 mm.
-
-
CBD can also be slightly dilated in patients post-cholecystectomy (after gallbladder removal).
Takeaway:
Always interpret CBD measurements in clinical context (age, symptoms, surgical history).
For an adequate gallbladder ultrasound scan, you should obtain:
-
Gallbladder long axis (sagittal) view
-
Includes the entire gallbladder, especially the neck, where stones often hide.
-
-
Anterior wall thickness measurement
-
Measured anteriorly to avoid artifact from posterior enhancement or bowel gas.
-
-
Gallbladder short axis (transverse) view
-
Confirms findings, evaluates for sludge/stones, ensures full visualization of the neck again.
-
-
Common bile duct (CBD) measurement
-
Required if gallstones are found, or if patient has abnormal LFTs or jaundice.
-
Helps assess for choledocholithiasis.
-
Correct answer: C — If the patient has a sonographic Murphy's Sign, then get a HIDA scan because this is a non-diagnostic ultrasound.
Explanation:
If the ultrasound is non-diagnostic (i.e., no stones, no sludge, normal wall thickness), but the patient has a positive sonographic Murphy’s sign, this raises strong suspicion for acalculous cholecystitis or functional gallbladder disease.
What is a sonographic Murphy's sign?
-
Maximal tenderness when pressing with the probe directly over the gallbladder
-
Highly specific for cholecystitis, especially when paired with clinical signs (fever, WBC elevation)
Next step: HIDA scan
-
A Hepatobiliary Iminodiacetic Acid (HIDA) scan assesses cystic duct patency and gallbladder ejection fraction
-
Used when ultrasound is inconclusive but suspicion remains
Why not the other choices?
-
A: Consult surgery — premature without more diagnostic clarity
-
B: Get HIDA scan (unconditionally) — only if clinical concern or positive Murphy’s is present
-
D: Discharge with elective referral — risky if the patient may have evolving cholecystitis
Correct answer: B — Curvilinear probe
Explanation:
The curvilinear (convex) probe is the preferred transducer for gallbladder ultrasound because:
-
It operates at 2–5 MHz, providing deep penetration needed to visualize abdominal organs like the gallbladder.
-
It offers a wide field of view, ideal for evaluating the RUQ.
Other options:
-
Phased array probe (A): Typically used for cardiac imaging; small footprint, less ideal for RUQ.
-
Linear transducer (C): High-frequency, used for superficial structures like vessels, soft tissue — not deep abdominal organs.
Correct answer: A — 3 mm
Normal Gallbladder Wall Thickness:
-
The normal cutoff is <3 mm when measured anteriorly on ultrasound.
-
≥3 mm is considered abnormal and may indicate:
-
Acute cholecystitis
-
Chronic cholecystitis
-
Other conditions like hepatitis, CHF, or hypoalbuminemia (non-specific)
-
Key Points:
-
Always measure the anterior wall, in a long-axis view.
-
Wall thickening should be interpreted in context — not all thick walls = cholecystitis.
Correct answers:
-
The posterior wall may be obscured by gallstones or sludge.
-
Posterior acoustic enhancement from the fluid-filled gallbladder can falsely inflate the thickness of the posterior wall.
-
The posterior wall may be obscured by adjacent bowel gas.
Explanation: Why Measure the Anterior GB Wall?
-
The anterior wall is closest to the probe, giving a clearer and more accurate measurement.
-
Artifacts like:
-
Posterior acoustic enhancement (brightening deep to fluid)
-
Shadowing from stones/sludge
-
Overlying bowel gas
can distort or obscure the posterior wall, making it unreliable for measurement.
-
Why?
-
Sludge (biliary sediment) can be seen in:
-
Fasting
-
Pregnancy
-
Critically ill patients
-
Normal patients without any pathology
-
-
It does not reliably indicate inflammation and is common in non-pathologic states.
Comparison of Specificity:
| Finding | Specificity for Acute Cholecystitis |
|---|---|
| Sonographic Murphy’s Sign | High — strong predictor when present |
| Pericholecystic Fluid | Moderate — often seen with inflammation |
| Gallbladder Wall Thickening | Low–moderate — nonspecific (seen in CHF, hepatitis, etc.) |
| Stone in Neck | Moderate–high — can obstruct cystic duct and trigger inflammation |
| Sludge | Low — least specific |
Why HIDA Scan?
-
A HIDA scan (Hepatobiliary Iminodiacetic Acid) evaluates cystic duct patency and gallbladder function.
-
It's the next best test when:
-
RUQ ultrasound is non-diagnostic
-
There is continued clinical suspicion (positive Murphy’s sign, RUQ pain)
-
-
CT abdomen/pelvis (CTAP) is not sensitive for cholecystitis and should not be first-line for isolated RUQ pain.
Why not the others?
-
Consult Surgery: Premature without diagnostic confirmation.
-
CTAP: Low yield for gallbladder disease.
-
Symptomatic control and reassess: Delays diagnosis, risky if patient has evolving cholecystitis.
Takeaway:
When RUQ ultrasound is inconclusive but clinical suspicion is high, proceed with a HIDA scan for definitive diagnosis.



























Comments
Post a Comment