Key Reasons for Choosing Nephrology (Part 1 Summary):
Complexity and Intellectual Challenge
Nephrology involves managing medically complex patients, which many find intellectually stimulating.
It allows for applying physiology at the bedside, especially renal and cardiac homeostasis.
Complexity is seen not as a barrier but as a fulfilling diagnostic and therapeutic challenge.
Breadth of Practice
Nephrologists care for critically ill ICU patients, manage chronic diseases like CKD, and oversee transplantation and dialysis.
The field blends acute high-intensity medicine with longitudinal primary care–like continuity, offering variety.
Strong Doctor-Patient Relationships
Nephrologists often follow patients over years through different stages of illness, including pre-dialysis, dialysis, transplant, and post-transplant.
These long-term connections are both emotionally rewarding and professionally meaningful.
Versatile Career Paths
Nephrology supports diverse roles: research, teaching, clinical care, administration, and work in industry (e.g., clinical trials, pharma).
Physician Identity
Nephrologists act as both specialists and primary care providers, coordinating care and managing comorbidities, especially in complex patients.
This dual role fosters a deeper engagement in all aspects of patient health.
Mentorship and Inspiration
Many were inspired by great teachers in medical school who effectively linked physiology with patient care.
The ability to connect science directly to clinical medicine is a hallmark of the field.
Impact on Patient Outcomes
Nephrologists can delay dialysis through proactive management and guide patients through successful transplantations, directly improving lives.
Not Just Dialysis
Although dialysis is visible, nephrology encompasses much more, including preventive strategies, chronic disease modification, and systemic care.
In essence, nephrology attracts those who value intellectual rigor, diversity of care, and meaningful, long-term relationships with patients—all while enjoying a wide range of career opportunities.
Part 3 Summary – Health Disparities & Nephrology
1. Nephrology Highlights Profound Health Disparities
A disproportionate number of dialysis patients are African American, Hispanic, Native American, or other non-Caucasian groups
Chronic kidney disease (CKD) thus reflects some of the most striking healthcare disparities in the U.S.
2. Opportunity to Address Disparities
Nephrology provides a unique platform for clinicians and researchers to explore the intersection of genetics, environment, socioeconomic factors, and healthcare access.
Physicians drawn to health equity, community health, and public health will find nephrology a meaningful field.
3. Research Potential in Understudied Populations
There's an urgent need for more clinical trials and population-specific research, including studies showing that interventions like aggressive blood pressure control may not have universal benefits.
Emerging genetic studies (e.g., APOL1 variants) are beginning to explain susceptibility in African Americans.
4. Nephrologists as Advocates & Policy Influencers
Many patients with CKD lack access to kidney-protective therapies, even when treatments are effective and affordable.
Nephrologists often witness systemic barriers firsthand and can become key advocates for healthcare reform and resource allocation.
5. Role in Prevention and Primary Care
Early diagnosis and preventive care—especially in underserved populations—is a critical unmet need in nephrology.
Nephrologists often act in a primary care capacity, managing comorbidities and ensuring continuity of care.
6. Personal and Professional Fulfillment
Caring for underserved populations not only provides academic and advocacy opportunities but also delivers deep personal fulfillment, especially for those who want to make a real-world impact on patients’ lives and communities.
Conclusion:
Nephrology is a powerful career choice for those passionate about health disparities, underserved care, and impactful clinical research. The specialty sits at the crossroads of science, service, and social justice, making it both a challenge and a calling.
Part 4 Summary – Misconceptions and Fulfillment in Nephrology
1. Medical Student Exposure is Skewed
Many trainees see only critically ill dialysis patients in hospitals, which can be discouraging and lead to a negative impression of nephrology.
This limited view misses the broad, rewarding spectrum of nephrology seen in outpatient settings, including long-term stable patients and transplant success stories.
2. Need to Showcase the Full Spectrum
Outpatient nephrology includes patients living full lives, such as working professionals with kidney transplants or patients with CKD managed successfully for years.
Training programs must do a better job of exposing learners to outpatient clinics, early CKD management, and thriving dialysis patients to combat misconceptions.
3. Opportunity for System-Level Impact
Nephrologists often feel frustration when late-stage patients arrive needing urgent dialysis, knowing earlier care could have prevented it.
However, this underscores nephrology’s potential for policy influence, prevention, and population health—especially regarding social determinants of health.
4. Dialysis is Life-Saving, Not Defeating
Dialysis is often unfairly stigmatized—yet it is a life-extending intervention for patients who would otherwise not survive.
Both chronic and acute dialysis provide hope, enabling some patients to eventually receive transplants or even thrive on long-term dialysis.
5. Innovations in Dialysis Care
Advancements like daily dialysis, portable machines, and individualized therapies improve patient quality of life.
Example: One patient traveled the U.S. in an RV while performing daily dialysis onboard—demonstrating the flexibility and evolving nature of modern dialysis.
6. Nephrologist Satisfaction is High
Despite initial perceptions, many fellows and practicing nephrologists report high career satisfaction once they experience the full scope and variety of the specialty.
The blend of lifesaving interventions, long-term relationships, intellectual challenge, and community impact makes nephrology uniquely rewarding.
Conclusion:
Nephrology is often misunderstood by trainees who only see its sickest patients. But in reality, it’s a field filled with hope, innovation, and deeply satisfying relationships. By broadening exposure and reframing dialysis as a triumph, not a tragedy, nephrology reveals itself as a vital, dynamic, and fulfilling career path.
Part 5 Summary – What Makes Nephrologists Enjoy Their Work
1. Variety and Flexibility
Nephrologists, especially in academic medicine, value the ability to do a mix of clinical care, teaching, research, and administration.
No two days are alike—this diversity prevents burnout and keeps the work intellectually and professionally engaging.
2. Long-Term Patient Relationships and Impact
Providing continuity of care is deeply rewarding, especially watching patients improve and live full lives over many years.
Helping patients understand and manage their own health brings daily meaning and satisfaction.
3. Teaching and Mentorship
Watching students and fellows develop enthusiasm for nephrology and have “lightbulb moments” is a highlight for many academic nephrologists.
Mentorship allows faculty to pass on knowledge and inspire the next generation of physicians.
4. Research and Knowledge Creation
Contributing to the field through innovative research and sharing discoveries at conferences like ASN is energizing.
Research allows nephrologists to expand their impact beyond individual patients, influencing broader practice and policy.
5. Administrative Roles as Tools for Broader Impact
Though often less glamorous, administrative work is reframed as an opportunity to support and enhance systems for better patient care, research, and education.
With experience, many find joy in enabling others to succeed, seeing faculty and institutional accomplishments as meaningful.
6. Making a Difference at Every Level
Nephrologists feel they improve the world daily—whether by helping a patient, mentoring a trainee, publishing new findings, or shaping institutional policies.
This multi-dimensional fulfillment is a core reason they continue to love and commit to their work.
Conclusion:
Nephrology offers a uniquely fulfilling career through its varied roles, deep relationships, educational impact, and research potential. For many, the specialty provides not just a job, but a calling to make meaningful change across multiple levels of healthcare.
Part 6 Summary – The Future of Nephrology and Final Reflections
1. Most Important Future Discovery: Early Detection & Prevention
The panel agrees that preventing kidney disease through early detection and public awareness will be the most impactful advancement over the next 20 years.
Chronic kidney disease (CKD) is a silent epidemic—often undiagnosed by both patients and primary care providers.
2. Personalized Medicine in Nephrology
There is a growing need to individualize care based on patient characteristics like race, gender, age, and genetics.
Current kidney-protective treatments may not work equally across all populations; tailoring interventions is key to improving outcomes and addressing health disparities.
3. Expanding Clinical Research
More prospective clinical trials are needed to verify which interventions work, for whom, and under what conditions.
Nephrology must invest in high-quality evidence generation to validate or challenge existing practices.
4. Improving Access and Application of Care
Advancements must be paired with equitable access—to care, medications, and follow-up.
Implementation science will be vital to apply new findings consistently and systemically across diverse populations.
5. Nephrologists Bridge Science, Practice, and Systems
Nephrologists are uniquely trained to translate science into clinical care, especially within structured systems like dialysis centers and CKD clinics.
Their systemic thinking also makes them effective administrators and leaders in health care delivery.
6. Final Reflections on the Career
All panelists express deep fulfillment from their choice to enter nephrology.
They cherish the variety, patient relationships, intellectual stimulation, and ability to improve lives through both preventive and life-saving therapies.
None of them regret the decision—calling it one of the best choices of their careers.
Conclusion:
The future of nephrology lies in preventing kidney disease, personalizing therapy, and ensuring equitable care. With its blend of science, service, and system-level thinking, nephrology remains a rewarding and forward-looking specialty for the next generation of physicians.
Part 7 Summary – Challenges, Gender Equity, and Flexibility in Nephrology
1. More Nephrologists Needed for Preventive Care
A key limitation in current practice is time constraints due to workforce shortages.
More nephrologists would allow greater focus on early interventions and prevention, rather than just tertiary or crisis care.
2. Gender Disparities and Underrepresentation of Women
Despite progress, fewer women choose nephrology compared to other specialties.
Possible deterrents include:
The perception that nephrology is difficult or not family-friendly.
Concerns about night/weekend call (e.g., emergent dialysis).
A lack of effective marketing of nephrology’s benefits to both men and women.
3. Embracing Part-Time and Job-Sharing Models
Resistance to part-time roles or job sharing, especially for women after training, is outdated.
Successful examples exist, showing continuity of care and job satisfaction are fully achievable with flexible models.
Flexibility is increasingly important to Millennials and dual-career families.
4. Broad Spectrum of Career Paths in Nephrology
Nephrology encompasses diverse practice models:
Outpatient CKD care
Inpatient/ICU nephrology
Transplant nephrology
Interventional nephrology
Administrative leadership
Medical ethics
Physicians can pivot roles as their personal and professional needs evolve.
5. Additional Avenues: Policy and Advocacy
The structure and reimbursement system around ESRD and transplantation positions nephrologists to influence:
Health policy
Legislative efforts
Systems-level reform
These opportunities expand nephrology’s impact beyond clinical care.
Conclusion:
To strengthen the future of nephrology, the field must:
Increase workforce capacity to prioritize prevention.
Promote flexibility and embrace evolving work-life balance values.
Address gender disparities through inclusive practices and messaging.
Highlight the broad, evolving opportunities nephrology offers—from direct care to public health leadership.
POCUS Quick Reference for Internal Medicine Residents
PELVIC ULTRASOUND
IUP = Gestational sac (GS) + yolk sac (YS) or fetal pole
Anembryonic pregnancy: GS ≥ 25 mm and no embryo
Interstitial ectopic pregnancy: Myometrial mantle < 7 mm
Pathologic free fluid: If anterior to uterus or >1/3 length of posterior uterus
Normal ovary: 3 × 2 × 1 cm
Tubal ring sign: Anechoic sac with echogenic wall separate from ovary → ectopic
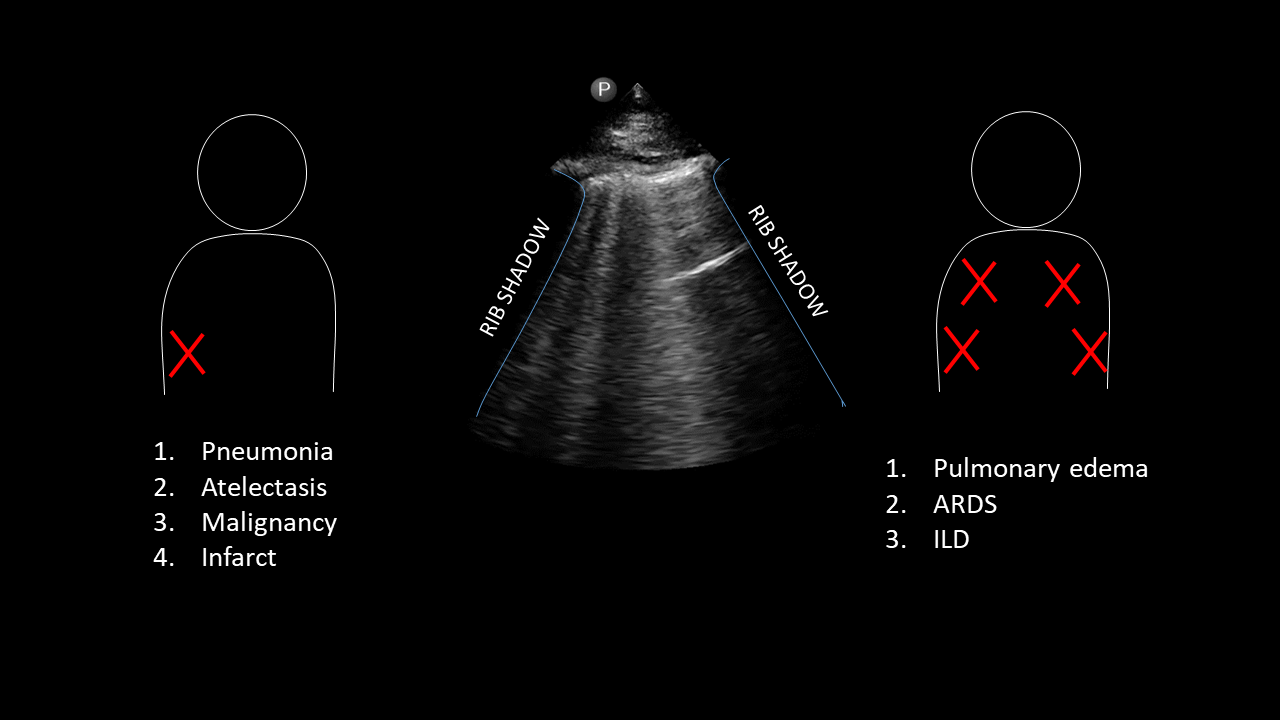
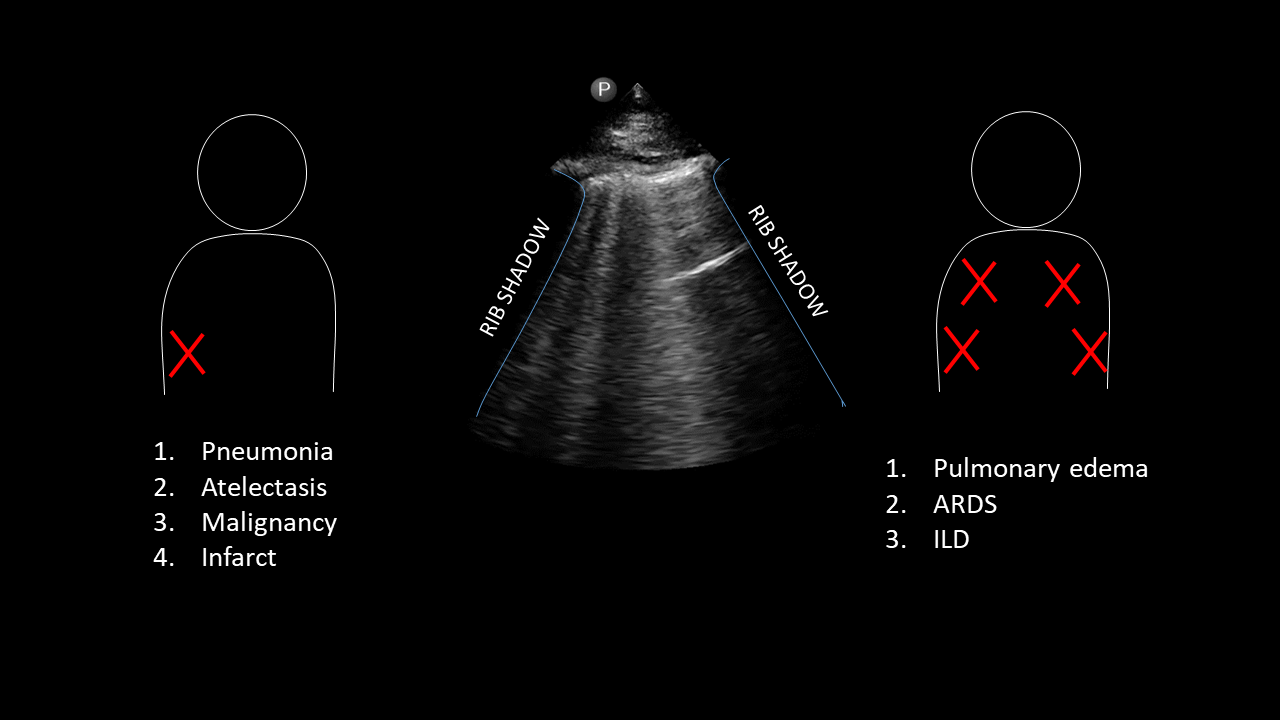
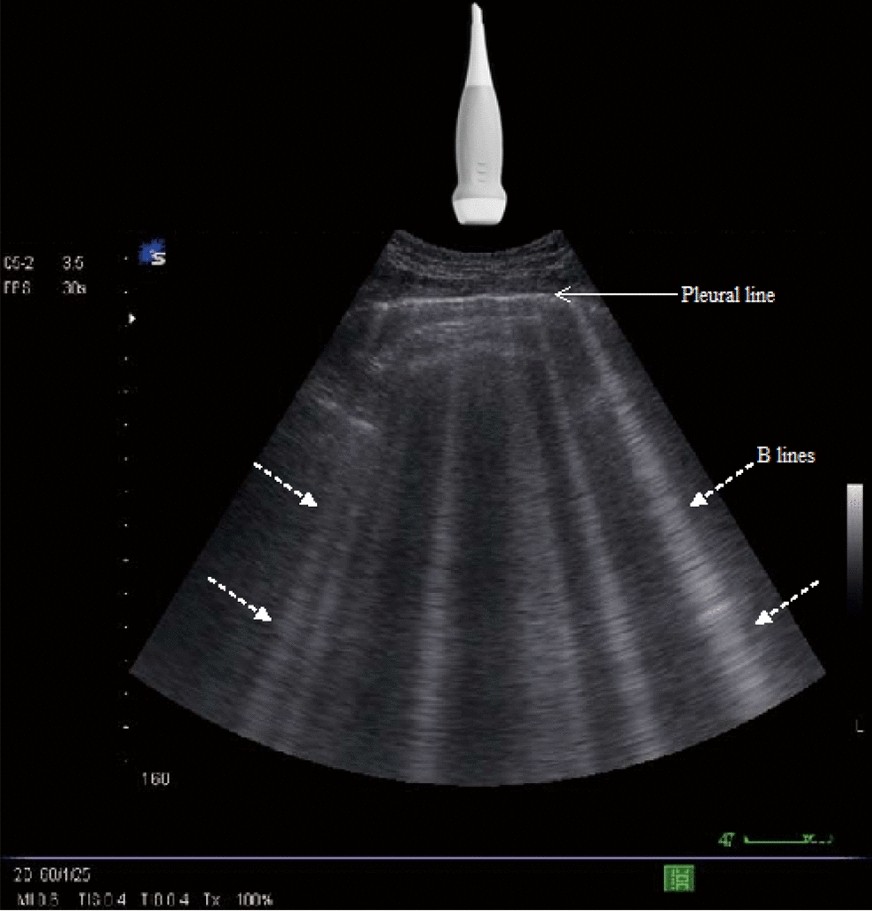
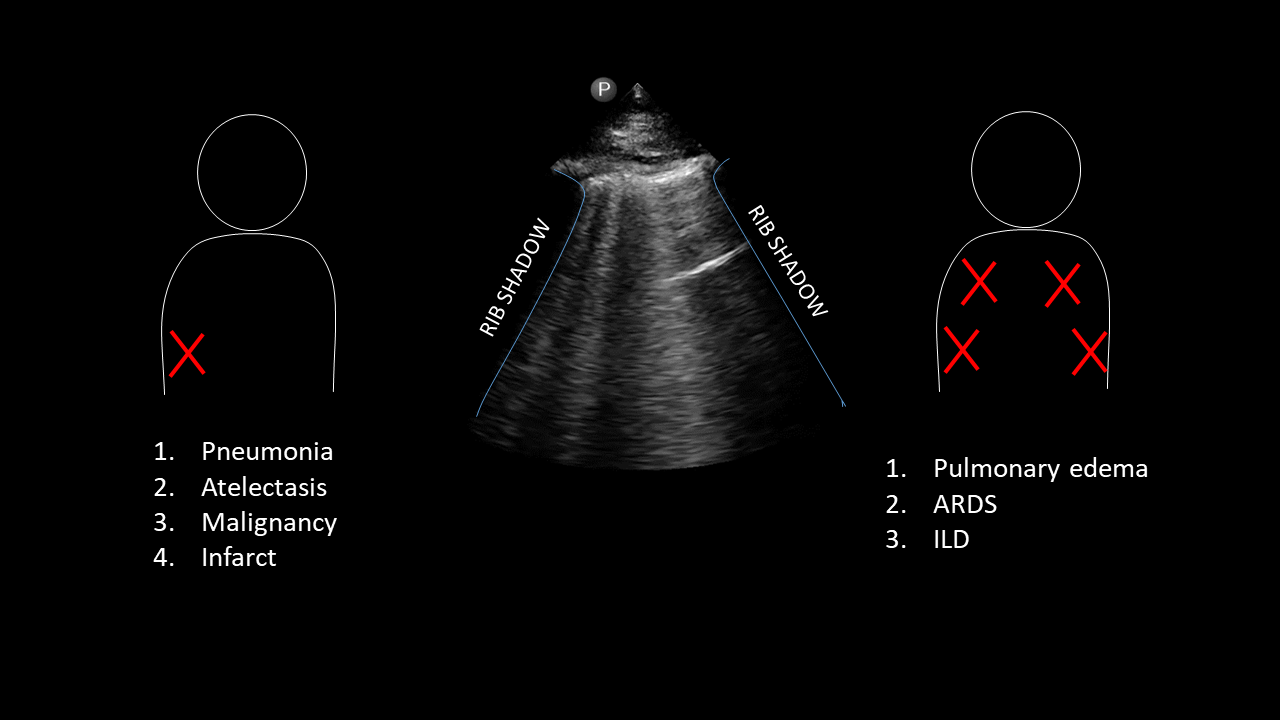
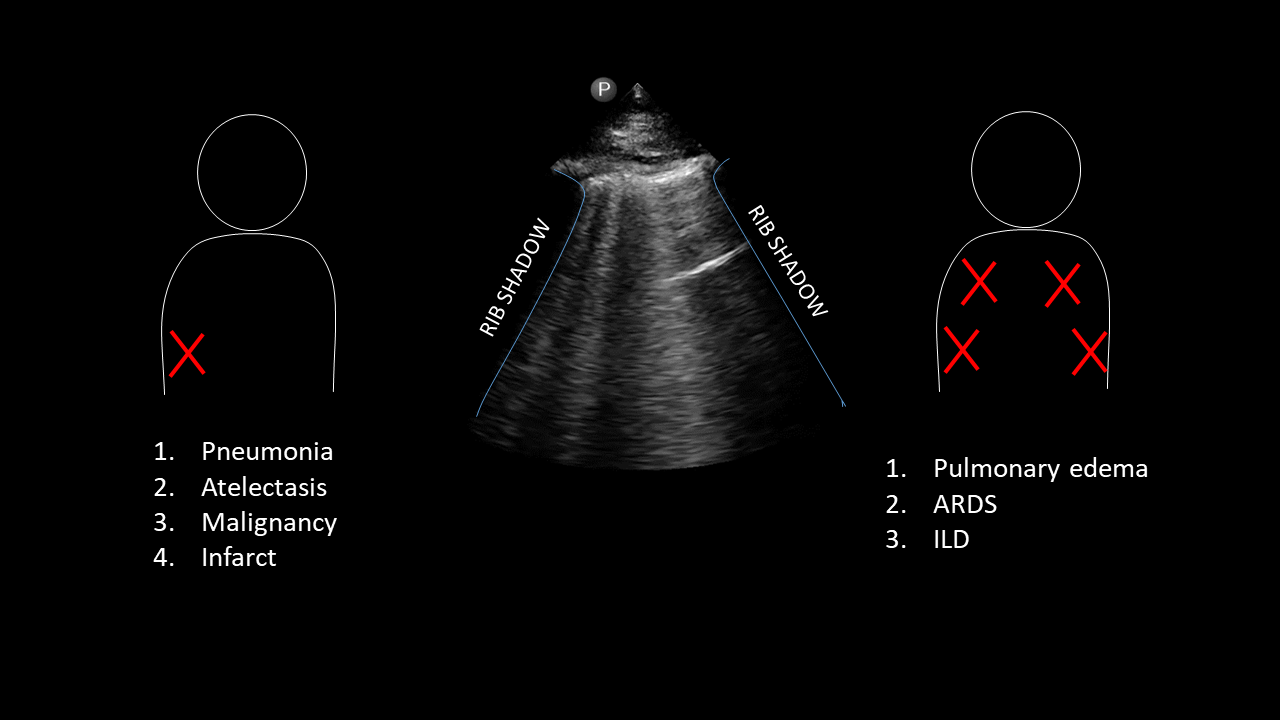
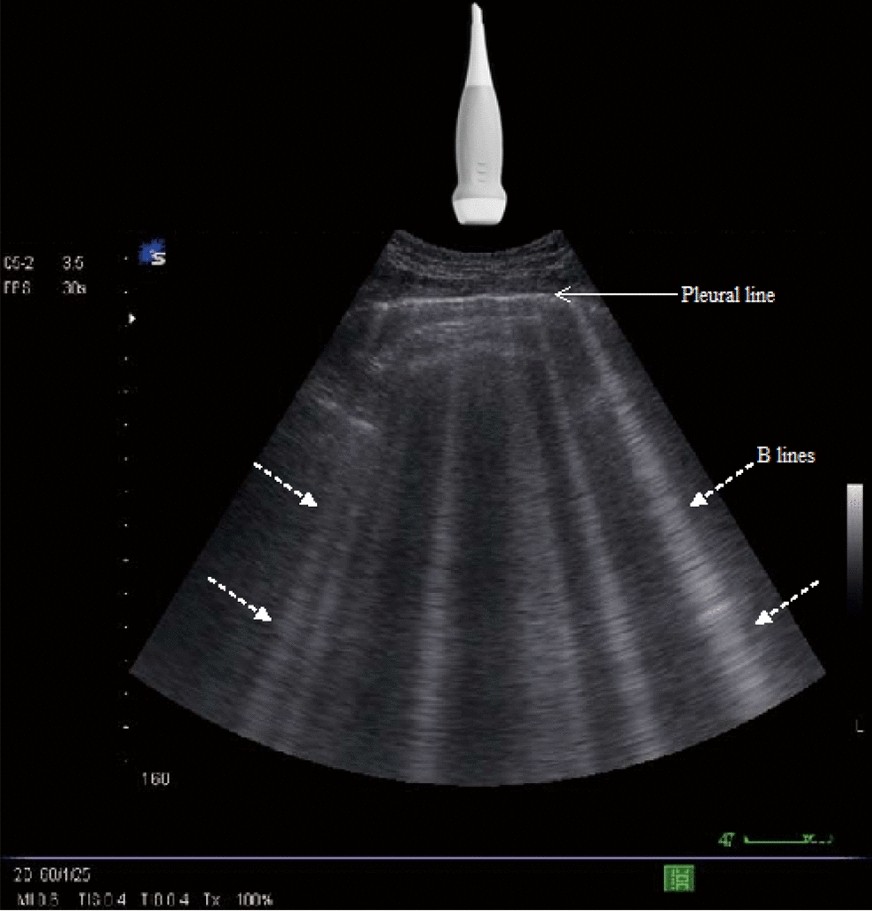
LUNG SIGNS
Lung point: 100% specific for pneumothorax
Hepatization of lung: Consolidation w/ bronchograms → pneumonia
Cobblestoning: Interstitial edema/cellulitis
CARDIAC
McConnell’s sign: RV free wall hypokinesia with hyperkinetic apex → PE
D Sign: RV pressure overload → flattening of septum on parasternal short
Views to capture (need 2 of 4):
Parasternal long (PSL)
Parasternal short (PSS)
Subxiphoid (SX)
Apical 4-chamber (AP4)
Absolutely — here’s the same list of key cardiac POCUS findings now with clear explanations of the physiology and clinical relevance behind each one. This will help you not only recognize the signs but also understand why they matter.
Detailed Guide to Cardiac POCUS Findings
EPSS (E-Point Septal Separation)
What it is: Measures the distance between the anterior mitral valve leaflet and the interventricular septum in early diastole using M-mode.
Why it matters: In healthy hearts, the mitral valve “snaps” open and nearly touches the septum due to robust LV filling. In systolic dysfunction, poor filling leads to reduced valve excursion.
Threshold:
Clinical context: Quick estimate of reduced systolic function; useful when global LV motion is hard to assess.
Aortic Root Diameter
What it is: Measured at the sinuses of Valsalva in PSL view during diastole.
Why it matters: Aortic root dilation may indicate risk of aneurysm or aortic dissection, especially in patients with connective tissue disease or chronic hypertension.
Threshold:
Left Ventricular (LV) Wall Thickness
What it is: Measures septal or posterior LV wall in diastole.
Why it matters: Thick walls suggest concentric hypertrophy, most commonly from chronic hypertension or aortic stenosis. Thickened walls can impair diastolic filling.
Threshold:
Right Ventricular (RV) Wall Thickness
What it is: Diastolic thickness of the RV free wall (best from subcostal view).
Why it matters: A thick RV suggests chronic RV pressure overload (e.g., pulmonary hypertension, chronic PE, COPD).
Threshold:
RV:LV Ratio (Apical 4-Chamber View)
What it is: Compares chamber sizes.
Why it matters: Normally the RV is smaller. RV dilation (RV:LV ≥ 1) indicates acute RV strain, often from a large pulmonary embolism or acute cor pulmonale.
Threshold:
Tamponade Physiology
Pericardial effusion: First finding on subxiphoid view or PSL
RA systolic collapse: Right atrial pressure is lowest during systole — it collapses first
RV diastolic collapse: RV can't fill against pericardial pressure
IVC plethora: Non-collapsible IVC suggests elevated RA pressure
Why it matters: These are classic signs of cardiac tamponade — a life-threatening condition requiring emergent drainage.
McConnell’s Sign
What it is: Akinesis of the mid-RV free wall with preserved apical contraction.
Why it matters: Highly specific (but not sensitive) for massive PE.
Mechanism: May relate to acute afterload mismatch and tethering of RV apex by the LV.
D Sign (Parasternal Short Axis)
What it is: Flattening or bowing of the interventricular septum during systole or diastole, making the LV look like a “D.”
Why it matters: Seen in RV pressure overload, such as in PE or severe pulmonary hypertension. The RV pushes into the LV and alters its shape.
Visual Estimate of LVEF
Clinical Tip:
Use multiple signs in context. For example:
EPSS ≥ 7 mm + poor wall motion → likely low EF
RV:LV ≥ 1 + McConnell’s sign + D sign → likely PE
Pericardial effusion + RA/RV collapse + plethoric IVC → likely tamponade
VASCULAR / DVT
Compressibility is key
Required compressions:
FAST (Focused Assessment w/ Sonography in Trauma)
AORTA
GALLBLADDER
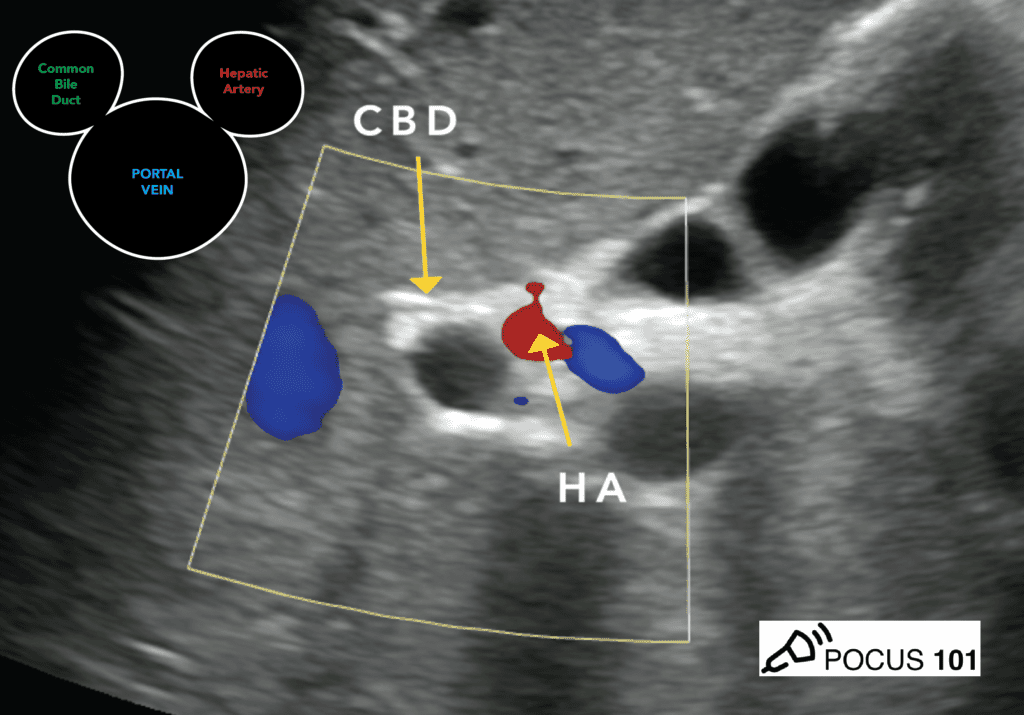
Required views:
Wall thickness < 3 mm
Common bile duct (CBD) < 6 mm
WES (Wall-Echo-Shadow) sign: GB full of stones
Double barrel sign: Dilated CBD with portal vein below
NEURO / OTHER SIGNS
Target Sign: Intussusception or appendicitis
Seagull Sign: Celiac axis and branches (hepatic/splenic)
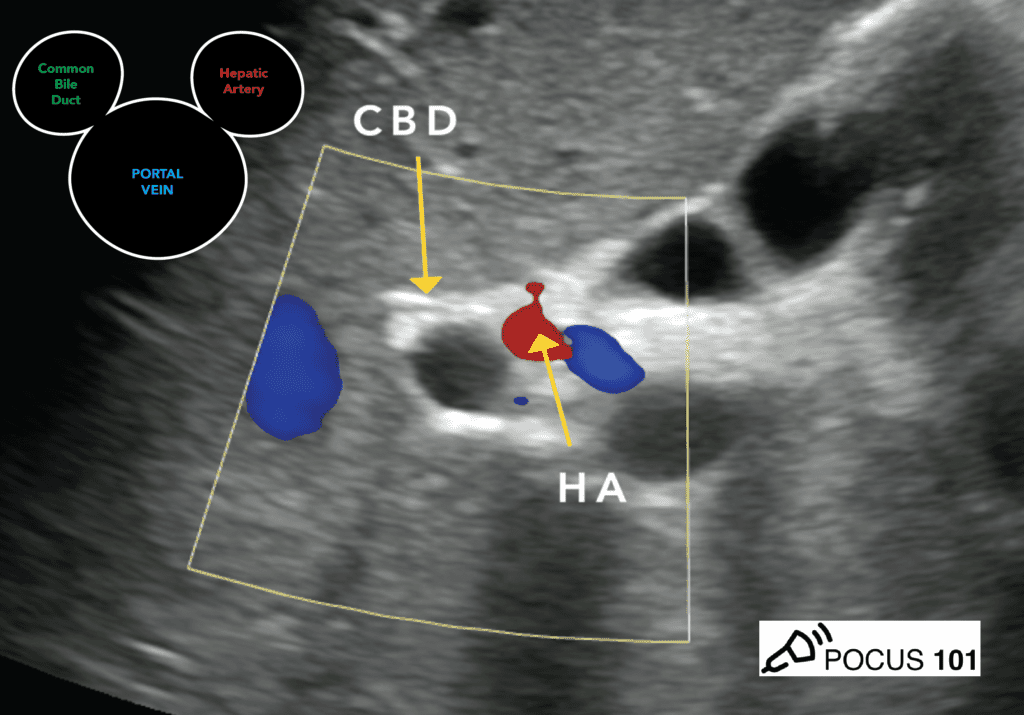
Mickey Mouse Sign: Portal triad: portal vein (face), hepatic artery + CBD (ears)
PROCEDURES (Need 5)
POCUS Tracking Reference for Internal Medicine Residents
LUNG
Log Requirement: 25 scans / 7 positive findings
Views (bilateral): Anterior, Midaxillary, Base
Edema: ≥3 B-lines per hpf bilaterally → Interstitial edema
OCULAR
CARDIAC
Quantitative Thresholds:
EPSS ≥ 7 mm → LVEF < 30%
Aortic root > 4 cm → Dilated
LV wall > 1.2 cm → LVH
RV wall > 5 mm → Chronic RVF
RV:LV ≥ 1:1 (A4C) → RV dilatation
Tamponade: Pericardial effusion + RA systolic collapse or RV diastolic collapse + non-collapsible IVC
RV strain: RV dilatation + D sign + McConnell's
IVC
Log Requirement: 3 scans
Views: Longitudinal or transverse, 2–3 cm distal to RA
Assess: Collapsibility + respiratory variation (M-mode or B-mode)
VASCULAR (Line/Access)
SOFT TISSUE
Log Requirement: 10 scans / 6 positive
Imaging: 2 planes + contralateral side for comparison
Look for: Cobblestoning, fluid, abscess
DVT
Log Requirement: 25 scans / 3 positive
Sites: Common femoral, saphenous, deep/superficial femoral, popliteal
Compressibility = Key
AORTA
Log Requirement: 25 scans / 2 positive
AAA: Outer wall to outer wall > 3 cm
Iliac aneurysm: Outer wall > 1.5 cm
Views: Proximal, Mid, Distal, Iliac bifurcation
RENAL
Log Requirement: 25 scans / 5 positive
Views: Kidneys + Bladder in both Sagittal and TV
Hydronephrosis = Positive
FAST EXAM
GALLBLADDER
PELVIC ULTRASOUND (TA and TV)
Transvaginal (TV): 10 scans / 4 positive
IUP = Gestational sac + yolk sac or fetal pole
Show: YS, FHR (use M-mode), Posterior cul-de-sac
EMM > 7 mm if <20 weeks
Transabdominal (TA): 25 scans / 14 positive
Uterus in two planes
Posterior cul-de-sac
Same thresholds for IUP
BOWEL
Appendicitis: Diameter ≥ 6 mm, non-compressible, blind end
Intussusception: Target sign, diameter ≥ 2 cm
Pyloric stenosis:
Muscle thickness > 3 mm
Canal length > 14 mm
SBO:
PROCEDURES
POCUS Flashcards – Set 1: Key Signs & Diagnoses
Q1: What confirms an intrauterine pregnancy (IUP)?
A1: Gestational sac + yolk sac or fetal pole
Q2: At what size is a gestational sac considered anembryonic?
A2: ≥ 25 mm with no embryo
Q3: What measurement suggests an interstitial ectopic?
A3: Myometrial mantle < 7 mm
Q4: What makes pelvic free fluid pathologic?
A4: If anterior to uterus or > 1/3 length of posterior uterus
Q5: Normal ovary size?
A5: 3 × 2 × 1 cm
Q6: What ovary size raises concern for torsion?
A6: ≥ 5 cm
Q7: What is the tubal ring sign?
A7: Anechoic sac with echogenic wall separate from ovary → ectopic
Q8: What is the WES (Wall Echo Shadow) sign?
A8: GB full of stones with shadowing
Q9: What is the “target sign” seen in?
A9: Appendicitis or intussusception
Q10: What does the “seagull sign” represent?
A10: Hepatic and splenic arteries branching off the celiac trunk
Q11: What is the “Mickey Mouse sign”?
A11: Portal triad: portal vein (face), hepatic artery & CBD (ears)

Q12: What is McConnell’s sign?
A12: Hypokinetic RV free wall with hyperkinetic apex (suggests PE)
Q13: What is the lung point?
A13: Edge of pneumothorax—100% specific
Q14: What does lung hepatization indicate?
A14: Pneumonia (consolidated lung with air bronchograms)
Q15: What does the D sign indicate on PS short view?
A15: RV pressure overload (flattened septum)
Q16: What is cobblestoning?
A16: Interstitial edema in soft tissue
Q18: What defines interstitial edema on lung ultrasound?
A18: ≥ 3 B-lines per hpf bilaterally
Q19: How many renal scans needed?
A19: 25 scans / 5 positive; kidneys and bladder in sag/TV
Q20: How many transvaginal pelvic scans are required?
A20: 10 scans / 4 positive; show uterus, posterior cul-de-sac, YS/FHR
Q21: What defines a normal endometrial stripe under 20 weeks?
A21: EMM > 7 mm
Q22: How many soft tissue scans required?
A22: 10 scans / 6 positive; 2 planes + compare contralateral
Q23: DVT scan requirements?
A23: 25 scans / 3 positive; compressibility of CFV, FV, popliteal
Q24: IVC scan requirements and findings?
A24: 3 scans; 2–3 cm from RA, assess with B/M mode for collapsibility
Q25: ONSD threshold for increased ICP?
A25: ≥ 5 mm (measured 3 mm behind globe)
Q26: EPSS ≥ 7 mm suggests what EF?
A26: EF < 30%
Q27: Aortic root > 4 cm means?
A27: Aortic root dilation
Q28: LV wall > 1.2 cm suggests what?
A28: Left ventricular hypertrophy
Q29: RV:LV ratio ≥ 1 in A4C suggests?
A29: RV dilation or RV strain
Q30: Signs of tamponade on ultrasound?
A30: Pericardial effusion + RA systolic or RV diastolic collapse + non-collapsing IVC
Q31: Criteria for AAA diagnosis?
A31: Aorta > 3 cm (outer to outer wall)
Q32: What diameter defines appendicitis?
A32: > 6 mm, noncompressible, blind tube
Q33: What defines pyloric stenosis?
A33: Muscle thickness > 3 mm, canal length > 14 mm
Q34: Gallbladder wall > 3 mm and CBD > 6 mm suggest?
A34: Cholecystitis (if with +Murphy, stones/sludge, pericholecystic fluid)
Q35: How many total procedure scans required?
A35: 5 total (e.g., paracentesis, thoracentesis, pericardiocentesis, LP)


From: Huang, Samuel
Sent: Tuesday, July 1, 2025 1:09 PM
To: Samuel Huang <samuelyhuang2023@gmail.com>; Samuel Huang <syh22@cornell.edu>
Subject: Pocus images
SYmptomatic UTI txt
3 populations renal tx in past month, invasive urologic procedures, or pregnant patients, stones, , children < 3 yrs and if recurrent require a renal+bladder US and VCUG. don't tx asymptomatic ppl even if they have foley catheter growing bacteria / fungi or diabetes
Txtmt for asx bacteriuria of pregnancy is nitrofurantoin / amoxicillin for 7 days. For pts w/ diabetes even if UA showing e coli 100K UA WBC > 10 w/ foul smelling urine don't txt
Postmenopausal women can be given estrogen to prevent UTIs as loss of estrogen causes dryness and irritations in the vagina and urethra making it more prone to infection.
Estrogen raises the lvls of health bacteria and helps tissues in vagina and urethra stay elastic and moist.
For uncomplicated cystitis the most common bugs are e. Coli, proteus, klebsiella, and staphylococcus saprophyticus and are treated otpt w/ fosfomycin x1d , bactrim x3d (kidney function), nitrofurantoin x5d (pulm fibrosis), ciprofloxacin x3d (qtc tendon tear), beta lactam 5-7d w/o need for c/s for inpt require IV ctx 1g for 1 day.
For complicated UTIs in addition to e. Coli proteus, klebsiella, staph saprophyticus you think serratia, morgenalla,
Zosyn needs EDTA and sodium citrate to work zosyn doesn't have it.
If zosyn if mixed with LR it precipitates
Cefepime is a good alternative, however cefepime does not have as broad of a coverage as zosyn
Bacteria isolated from ascitic fluid in 519 patients with spontaneous bacterial peritonitis
Organism | Percent of isolates |
Escherichia coli | 43 |
Klebsiella pneumoniae | 11 |
Streptococcus pneumoniae | 9 |
Other streptococcal species | 19 |
Enterobacteriaceae | 4 |
Staphylococcus | 3 |
Pseudomonas | 1 |
Miscellaneous* | 10 |
*In some regions of the world, such as Korea, Aeromonas hydrophila infection is an important cause of SBP, particularly in warm weather months. Affected patients commonly also have diarrhea. [Choi JP, et al. Clin Infect Dis 2008; 47:67.]
Data from McHutchison JG, Runyon BA. Spontaneous bacterial peritonitis. In: Gastrointestinal and Hepatic Infections, Surawicz CM, Owen RL (Eds), WB Saunders, Philadelphia 1995. p.455.
Graphic 80188 Version 3.0
© 2024 UpToDate, Inc. and/or its affiliates. All Rights Reserved.
EKSOESPM
E coli, klebsiella, streptococcus species, other streptoccocal enterobacterciae, staphylococcus aureus, pseudomonas, miscellanous
Ascitic paracentesis
Cultures, cell count, pmns, albumin, protein, SAAG
Serum protein
34,000 RBCs mesothelial cells
Stanford Medicine 25 teaches and promotes bedside medicine exam skills to students, residents and healthcare professionals both in person and online. stanfordmedicine25.stanford.edu |
Nontraumatic subdural hemorrhage

Questions to Answer
TTE / TEE?
Anticoagulate Heparin gtt? what is the threshold to discontinue.
Broncho / no Bronch
TEE for Afib [3][9][32]
Goals
To evaluate for thrombi and reduce the risk of thromboembolic events
Visualize the atria and the left atrial appendage (hotspots for thrombogenesis)
Indications (prior to cardioversion)
New-onset Afib or atrial flutter of ≥ 48 hours or unknown duration
No previous anticoagulant use or subtherapeutic anticoagulation
High stroke risk (e.g., history of stroke, left atrial thrombus, HOCM, or rheumatic fever)
Interpretation
No thrombus identified: Safe to proceed with rhythm control
Thrombus identified: Anticoagulate for ≥ 3 weeks and consider repeat TEE prior to attempting rhythm control.
currently in atrial fibrillation
SINUS TACHYCARDIA WITH PREMATURE SUPRAVENTRICULAR COMPLEXES
RIGHT ATRIAL ENLARGEMENT
ST & T WAVE ABNORMALITY, CONSIDER INFERIOR ISCHEMIA
ABNORMAL ECG
CTAPA
There is mild enlargement of the pulmonary arteries. There is new thrombus within the left atrial appendage
Problem with CTAPA is that we do not know if picture is resting or contracting ventricle.
TTE / TEE?
If this is afib we would not do TEE.
In left atrial appendage do we anticoagulate with heparin?
Intracardiac Embolism 15- 20 percent of strokes.
Question becomes Should we do a TEE?
Why TTE over TEE?
TEE is more invasive.
This patient has Acute respiratory distress Requiring Hi flow 100% now 90%.
Such a high FiO2 requirement may not be considered Medically optimized for emergent TEE.
TTE is chosen in individuals
1. > 45 years w/ neurologic event
2. abrupt occlusion of major peripheral or visceral artery
3. High suspicion of LV apical thrombus
4. patients in whom TEE is contraindicated (esophageal stricture), unstable hemodynamic status
TEE
We choose TEE as the initial test to localize the source of embolism in the following circumstances:
-Patients <45 years without known cardiovascular disease (ie, absence of infarction or valvular disease history) for whom a patent foramen ovale is strongly suspected.
-Patients with a high pretest probability of a cardiac embolic source in whom a negative TTE would be likely to be falsely negative.
-Patients with atrial fibrillation and suspected left atrial or left atrial appendage thrombus, especially in the absence of therapeutic anticoagulation, and presuming information from the TEE would impact management (eg, cardioversion is desired).
-Patients with any prosthetic heart valve.
-Patients with suspected aortic pathology.
Patient meets the above criteria.
83F PMHx ILD / COPD / Afib on eliquis / PE in 2005 found to be in Severe Acute respiratory distress syndrome requiring hi flow 90%FiO2 found to have a left atrial appendage thrombus on heparin gtt.
Pink frothy sputum on admission. Patient only reported 1 blood tinged episode.
May not be NSTEMI. TnI 0.073 -> 0.124 w/ Sinus tach pvcs 113 possible TWI II, III, AVF blood pressures sometimes dropping to MAP 68 was once brady to 56 sometimes tachy to 119.
Cardiac
Thrombus
Left ventricle
Prior myocardial infarction
Dilated cardiomyopathy with reduced cardiac output
Left atrium
Atrial fibrillation or atrial flutter
Mitral stenosis
Cardiac amyloidosis
Prosthetic valve (mitral or aortic) thrombus
Systemic venous or right heart thrombus with paradoxical embolization via right-to-left intracardiac shunt
Atrial septal defect
Patent foramen ovale
Atrial septal aneurysm
Nonthrombotic masses
Tumor
Myxoma
Papillary fibroelastoma
Vegetation
Infectious endocarditis
Noninfectious (marantic) endocarditis
Underlying malignancy
Systemic inflammatory disease (ie, SLE, RA)
Sepsis
Severe burns
Mitral annular calcification
Aortic
Complex atheroma (protruding >4 mm, mobile component, and/or plaque ulceration)
Antithrombotic Therapy (Stroke 2010;41:2731)
Treatment recommended for all pts except those with CHADS2-VASc 0, lone AF episode, or contraindications to therapy.
LA appendage is the source of at least 90% of thrombi in pts with CVA and AF.
Subclinical AF still associated with increased stroke/systemic embolism(ASSERT).
Patients at relatively low risk for thromboembolism may be maintained on ASA alone (see below), but no reliable data
exist to guide decision between 81mg vs. 325mg ASA dose
Left atrial thrombus management - LAAT
Anticoagulation mainstay of stroke prevention in patients with atrial fibrillation which is a common cause of LAAT
TEE crucial to exclude LAAT before procedures such as pulmonary vein isolation and Left atrial appendage occlusion
Does she have contraindication to anticoagulation, do we need to use a left atrial appendage occlusion device such as a watchman? implanted percutaneously to seal the left atrial appendage and reduce risk of thromboemblism
she is in sinus rhythm no need for cardioversion.
Also, cardioversion should only be used after documented period of effective anticoagulation to reduce the risk of thromboemblism.
People with atrial fibrillation and history of left atrial appendage thrombus may need lifelong anticoagulation.
Procalcitonin
This is how I used procalcitonin before.
Trend procalcitonin. Can trend daily. Procalcitonin < 0.25 discontinue antibiotics
Even in ESRD has still some value just harder to interpret imo there's no harm in getting procalcitonin because you get it with morning labs
This 0.25 cut off is based on reducing antibiotic usage in individuals with Ventilator associated pneumonia:
Procalcitonin determination significantly increased the number of antibiotic free-days alive 28 days after VAP onset (13 (2-21) days versus 9.5 (1.5-17) days). This translated into a reduction in the overall duration of antibiotic therapy of 27% in the procalcitonin group (p = 0.038). After adjustment for age, microbiology and centre effect, the rate of antibiotic discontinuation on day 28 remained higher in the procalcitonin group compared with patients treated according to guidelines (hazard rate 1.6, 95% CI 1.02-2.71). The number of mechanical ventilation-free days alive, intensive care unit-free days alive, length of hospital stay and mortality rate on day 28 for the two groups were similar.
From this source:
Stolz D, Smyrnios N, Eggimann P, Pargger H, Thakkar N, Siegemund M, Marsch S, Azzola A, Rakic J, Mueller B, Tamm M. Procalcitonin for reduced antibiotic exposure in ventilator-associated pneumonia: a randomised study. Eur Respir J. 2009 Dec;34(6):1364-75. doi: 10.1183/09031936.00053209. Epub 2009 Sep 24. PMID: 19797133.
A procalcitonin-guided strategy to treat suspected bacterial infections in non-surgical patients in intensive care units could reduce antibiotic exposure and selective pressure with no apparent adverse outcomes.
Patients in the procalcitonin group had significantly more days without antibiotics than did those in the control group (14.3 days [SD 9.1] vs 11.6 days [SD 8.2]; absolute difference 2.7 days, 95% CI 1.4 to 4.1, p<0.0001)
Source
Bouadma L, Luyt CE, Tubach F, Cracco C, Alvarez A, Schwebel C, Schortgen F, Lasocki S, Veber B, Dehoux M, Bernard M, Pasquet B, Régnier B, Brun-Buisson C, Chastre J, Wolff M; PRORATA trial group. Use of procalcitonin to reduce patients' exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet. 2010 Feb 6;375(9713):463-74. doi: 10.1016/S0140-6736(09)61879-1. Epub 2010 Jan 25. PMID: 20097417.

Morphine is bad for kidneys
It gets metabolized into
Glucuronide conjugation to 3, 6
Metabolites accumulate in renal failure and cause toxicity
Morphine 3 and morphine 6 glucuronide
Right 13-15
Left 17-19
Better to go deeper first then pull back
Look at monitor for PACs.
backwards

KPOT trial
Mannitol discontinuation for uosm>320
PMID 32227294 2020 Guidelines for the Acute Treatment of Cerebral Edema in Neurocritical Care Patients
Clinicians commonly use a serum osmolarity of 320 mOsm/kg or an osmolar gap of 20–55 mOsm/kg to estimate the risk of AKI with mannitol; both are indirect surrogates of serum mannitol concentration [91]. Serum mannitol concentration is possibly the best indicator of AKI risk based on animal models, however most clinical laboratories are not able to directly measure this
Bicarbonate therapy is not recommended in children with DKA unless pH falls below 6.9 because of the association between bicarbonate treatment and cerebral edema.
wound care orders
Local lower as tolerated right, patient to be weightbearing as tolerated to right lower extremity in a surgical shoe at all times please cleanse the wound with normal saline extremity tissue with BetadineTo the hospital psych follow-up at at 125 pressure mmHg continuously change dressings 3 times weekly cefazolin clean dry and intact between dressing changes
Silicone foam dressing (mepilex)
Lorazepam 4mg repeat once in 5-10 minutes
2mg then give more. Start with 2
Midazolam no IV access 0.2mg/kg IV max 10mg, utilize IM if no IV access
Load
If past 5 minutes
Status load something
More popular medications
ESETT - established status epilepticus treatment trial
Valproate, keppra, phenytoin
Cardiac arrhythmias - fosphenytoin, phenytoind
Seizing 20-40 minutes
Intubating verside /
1500 IV
Make bag on the spot
ED 1500, then another 1500
versed
Adults 5-10
Inducers affect the doacs
Load give fosphenytoin
Maintenance to phentyoind
Max 1.5g
Maintenance 100mg IV TID
Osteoporosis, gingival hyperplasia, atrophy
depakote
Status load
40mg/kg max 3g, with meropenem vpa lowered in 1-2 days
May need meropenem
Increase lamotrigine levels need to decrease and monitor lamotrigine levels
Hard to tell if encephalopathic
½ is dialized need post HD dose
irritability
Newer cousin riveracetam more selective and less mood side effects
Status 300-400mg maybe 200 if 40kg. Avoid if 2nd / 3rd degree AV block
NES - nonepileptic seizures
pseudoseizures
10% of epilepsy patients
Co-morbid w/ epilepsy mood disorder
NES manifestations
Out of phase limb movement
Asynchronous jerk between L and R extremities
Tremors, threashing
Pelvic thrusting
Seen in epileptic seizures
Eye closure, forceful eye closure
80-90% of epileptic seizures eyes are open
\80-90% nonepileptic seizures eyes are closed
Variable <2mm open half the time for epileptic
Closed for nonepileptic
Tonic clonic
Tonic - stiff discharges slow down rhythmic twitching
Fast phase and slow relaxation phase
Nonepileptic seizures, side to side movement
Tonic clonic
Abdomen is tight.
Nonepileptic moaning groaning, hyperventilating flushed and pale.
Drowsy GTC, alertness convulsive PNES
Thermal burns
Post ictal
Gtc
Lacosamide (LCM) VIMPAT
Switch
Samuel Y Huang MD
PGY-2 Internal Medicine
Icahn School of Medicine
Mount Sinai South Nassau
One Healthy Way
Oceanside, NY 11572
(732) 289-8008
From: Huang, Samuel
Sent: Monday, February 10, 2025 1:42 PM
To: samuelyhuang2023@gmail.com <samuelyhuang2023@gmail.com>
Subject: Epilepsy monitoring Unit
Camera on ceiling to get bird's eye view see what the seizures look like, what they look like on video, gradually titrate off of medications.
MSW, MSH
Get episodes differentiate psychogenic non epileptic seizures
Establish when fall of rails
Presurgical work up if they are surgically resistant
Beta alpha theta delta
Occipital lobe, central lobes, mu rhythm goes away if you move
Beta rhythm faster awake at rem
If they get benzodiazepines or barbiturates
Mildly encephalopathic, slow, lethargic. Focal slowing
Focal dysfunction, post ictal structural lesion
Persistent, continuously low, structural lesion
Focal epileptiform
Epileptiform, hyper
Focal sharp waves
Interictal discharges - sharp waves seen in between the seizures
6 square centimeters
Measures currently extracellular outflow
Sharp and slow waves, child absence seizures.
EMG / muscle artifact bigger and more conlufence. Up straight up and down. Muscles faster than the nerves. Pulse artifact ballismic, if EEG on the temporal artery. Lines up with T.
Middle bigger wave, vertex wave - benign finding during stage 1 and 2 sleep.
Wider looking sharp looking spikes.
Eeg reports outside hard to trust other people's reads. Questionable seizure history, fainted.
capture.
Europe 50 hz
Wicket spikes - drowsiness and sleep
Rhythmic mid temporal benign discharges, spikey and sharp
Psychomotor variants
Until in psych patients
GRDA - generalized rhythmic delta activity - increased intracranial pressure, thalamic lesion. Not associated with increased risk of seizures.
Indicative of risk for seizures, rhythmically slow
Small piece of seizure. Similar to seizures in the past. Think about increasing medications.
IIC 1->2.5 hz of sharp waves over 10 seconds doesn't mean seizures but means close to a seizure and treated like seizures
Seizures increase risk of injury during seizures, aspiration, NYS law cannot drive for 1 year, NJ law 6 months but mandated reporting, quality of life, chronic memory
NJ 6 months but mandates reporting
State by state, ambiguous
Rare circumstances, chances of repeat seizure are low.
Over the years, many new medications
Keppra - third generation drug.
ASM - anti-seizure medications
ASMs - 66% 2/3 seizure meds
Resection 2/3-75%
Neocortical
Seizure freedom, if you can't resect, resect lateral connections
Prevent drop seizures
Three FDA approved devices.
Partial vs primary generalized
Comorbid conditions, drug interactions
Focal versus primary generalized
Epilepsy - spikes everywhere at once
Focal epilepsy from stroke / tumor
Medications for focal epilepsies that worsen others
IV versus PO version
Take into consideration elderly and pregnant
Broad spectrum - generally used - clobazem, lamotrigene, keppra, topiramate, valproate
Narrow spectrum
absence
Lacosamide
Ethosuximide absence seizures
Asm - antiseizure meds
Keppra SV2a vesicle receptor protein, help vesicles merge with protein into membranes.
Valproate sodium channel and gaba
Status epilepticus
Focal status epilepticus w/ impaired consciousness after 10 minutes
One arm is changing. Don't have to freak out until after 10 minutes
Stabilization phase
ABCs - airway,
Make sure patient is not hypoglycemic
IV thiamine before the dextrose.
Alcoholic, thiamine deficiency not a lot of sugar, get wernicke
Body is tonic / clonic
Initially phase 1mg/kg 4mg adults so heavy
















Comments
Post a Comment